Many types of tests are used to help diagnose bile duct cancer. These can be grouped as radiology, serology, and pathology.
Radiology Tests ▼
1. Ultrasound
An improvement on the standard (transabdominal) ultrasound.
Ultrasonography of the liver and gallbladder is usually the first radiologic study used to evaluate jaundice or right-upper quadrant (abdominal) pain. During standard ultrasound the probe is placed externally on the abdomen which limits the resolution of the images. Ultrasound often detects large gallbladder cancers, but often misses smaller extrahepatic bile duct cancer. Standard CT images are often not optimal for diagnosing subtle abnormalities in the bile ducts and other organs. EUS is an improvement of this technique.
Procedure:
For an EUS, the ultrasound probe is placed in close proximity to the bile ducts by attaching it to the end of a standard gastrointestinal endoscope and passing the scope in the mouth, down the esophagus and into the stomach and duodenum . This produces a much clearer image than a transabdominal ultrasound.
Accuracy:
- EUS enables the investigator to identify abnormalities 1 cm or larger. There are small bile duct cancers that can be detected with EUS that cannot be visualized currently with a CT scan. Technological improvements are enabling a generation of more accurate images of the bile ducts and such improvements are expected to continue.
- It is the most accurate method for detecting the spread of cancer to the portal vein (not as accurate for arterial involvement).
- EUS will visualize masses of less than 1 cm but often will not be able to determine whether the mass is a cancerous. Fine needle aspiration done in conjunction with EUS may overcome this limitation.
- The main variable in the success of an EUS investigation is the experience of the endoscopist. The technique is difficult and the optimal use of this technique depends on the considerable skill of the endoscopist. Many centers now have endoscopists trained in the technique, but EUS is still not available at all medical centers.
Risks:
When done in conjunction with FNA there is a low risk of complication, 5 out of 124 patients 1.1%), all non-fatal complications. Fever, inflammation, perforation of duodenal or esophageal wall, hemorrhage of cystic tumor.
2. Computed Tomography (CT)
Scanning, which is essentially a detailed X-ray delineation of the body, is more sensitive for detecting both gallbladder and bile duct cancers.
3. MRI
Magnetic Resonance Imaging is becoming more sensitive than CT scanning, is less invasive and is slowly becoming more popular. CT and MRI have the added benefit of detecting enlarged lymph nodes near the tumors, which can suggest that a cancer has spread (metastasized) to the lymph nodes.
4. Endoscopic Retrograde Cholangio-Pancreaticography (ERCP)
Cholangiography, which involves the injection of a radioopaque dye into the biliary system, is the procedure of choice for determining the extent of tumor in the biliary tract. The procedure is done either through the skin (Percutaneous Transhepatic Cholangiography-PTC) or through an endoscope fed through the esophagus and into the duodenum.
During this procedure an X-ray is taken of the pancreatic duct and bile ducts. These ducts drain secretions from the pancreas and liver respectively. Obtaining such pictures requires that an endoscope be placed in the mouth through the esophagus and stomach, then into the duodenum.
Procedure:
The patient is sedated and given potent pain relievers (opiate) after on overnight fast. A local anesthetic is sprayed to the back of the throat. Frequently, muscle relaxants are used to relax the duodenum and ampulla (an anticholinergic drug, or glucagon, nitroglycerin). During the test patients are monitored to ensure that they are not over sedated. The monitoring includes a pulse oximeter (a probe fastened to the patient's finger that measures blood oxygen concentration) and a heart rate monitor. During the ERCP, the degree of sedation is much greater than that used for an EGD, so often the patient is asleep.
Using a modified endoscope, the investigator visualizes the duodenum on a monitor and finds the small opening where the bile duct and pancreatic duct empty into the duodenum (the ampulla of Vater). A thin catheter is passed through an opening in the endoscope and through the ampulla. Once the catheter has been placed through the opening (cannulated), a dye is injected into the pancreatic and bile ducts. This enables images of these ducts to be obtained. X-rays are taken of the abdomen over the area of the bile ducts and gallbladder and are examined on screen by the attending physicians.
Despite the medication, occasionally the patient may feel discomfort and may retch. If discomfort occurs additional pain relief is usually provided. Symptoms arising from complications may also rarely occur.
Accuracy:
Will show the indirect effects of bile duct cancer such as blockage or dilatation of the ducts and inflammation of the tissue. Similar symptoms can be caused by conditions such as chronic pancreatitis, sclerosing cholangitis, or stones in the pancreatic or bile ducts. By examining the pattern of these changes, it is possible to predict with a high degree of certainty if an abnormality is a cancer.
An ERCP can detect an abnormality suspicious of cancer in about 9 out of 10 patients who are investigated for possible adenocarcinoma. Patients who have very small cancers, less than 2 cm, that currently do not alter the main ducts of the pancreas or the bile duct will not be visible.
Occasionally, it can be very difficult to tell if an abnormality in the bile duct is due to cancer or inflammation. Tissue biopsy provides confirmation of the presence of cancer
Results:
If the test results are abnormal, a sample of biliary fluid from the bile duct or a sample of tissue by biopsy can be obtained if necessary. This can be done either during the ERCP by positioning a biopsy forceps while looking at it on screen. Alternatively, the fluid or tissue sample can be obtained by visualizing the are of concern using other imaging techniques and performing a needle biopsy (FNA).
As a Treatment:
Most importantly, if a bile duct cancer is present and the patient is not a candidate for curative surgery, therapeutic procedures can be performed using ERCP. These procedures can provide considerable relief for the patient with minimal inconvenience or risk. Bile duct cancers frequently block the bile duct that prevents the proper flow of bile from the liver. The therapeutic intervention typically alleviates symptoms caused by duct blockage such as jaundice, generalized and progressive itching, liver damage, inadequate digestion of food, a risk of bacterial infection of the blood and severe pain. Placing a stent into the bile duct to allow bile drainage can extend an individual's life and improve their quality of life. The patient does not feel the presence of the stent in their bile duct or pancreatic duct.
Risks:
The main complications of the ERCP as a diagnostic procedure are pancreatitis, infection and bleeding.
The insertion of a therapeutic stent can have complications such as bleeding, inflammation of the pancreas (pancreatitis), bile duct damage and leakage, and infection. Bleeding and pancreatitis is more likely if a large (wide-bore) stent is placed as it requires a cut to be made to enlarge the opening of the narrow ampulla where the bile and pancreatic fluid enters the duodenum (see figure). The cut primarily targets a small sphincter muscle surrounding the ampulla (hence, the procedure is termed a sphincterotomy).
Overall, less than 1 in 10 individuals will have such a complication and severe life-threatening complications are rarer (1-2%). The risk of a complication when a sphincterotomy is not performed is less (2-5%) and depends on the number and size of the stents inserted. Usually therapeutic ERCP can be done as a same day procedure without the need for an overnight hospital stay. If complications occur or are suspected hospitalization might be required. Biliary stents usually succumb to blockage after several months as a result of further cancer growth. This may require periodic stent replacement.
There is also a small risk of an allergic reaction to the dye, which contains iodine. Rarely, drugs used to relax the ampulla of Vater can have side effects such as nausea, dry mouth, flushing, urinary retention, rapid heart rate (sinus or supraventricular tachycardia), or a drop in blood pressure.
Serology Tests ▼
CA19-9
Serology refers to measurements of serum substances (markers) present in the blood which may predict the presence of tumor. The most commonly used marker is the serum CA19-9, which tends to be elevated in patients with bile duct cancer. However, this marker is not specific to bile duct cancer. It can be elevated in patients with other types of cancer and in patients without cancer. It is therefore not a very good screening test for the general public.
This is a tumor marker for bile duct cancer that is measured through a blood test. It is useful in assisting with an initial diagnosis. However, it is more useful in measuring the effectiveness of cancer treatment by studying the patient's CA19-9 levels over time.
In general, before surgery, the higher the CA19-9 level is (normal CA 19-9 level is 40 units per milliliter), the larger the tumor is and the less chance that the tumor is resectable. For the purposes of evaluating treatment, a decreasing or stable CA19-9 level generally indicates an improved prognosis and an increasing level indicates the progression of disease.
Currently, there are not sufficiently accurate diagnostic blood tests for bile duct cancer. Very few cancers, such as prostate and liver cancers, can be confidently diagnosed solely on the basis of blood test results. Perfecting a suitable blood test for bile duct cancer is an area of active research because it would enable screening for individuals considered at-risk.
Accuracy:
CA19-9 is elevated in the blood of about 90% of individuals with bile duct cancer. Other blood tests such as CEA can be used in combination with CA 19-9 to improve the accuracy of the test. Supplemental imaging studies and tissue samples are required with CA19-9 levels for a definitive diagnosis.
CA19-9 can be used to track treatment progress of previously diagnosed bile duct cancer patients. This blood test in conjunction with periodic CT scans will show whether the cancer is in remission or is continuing to grow.
Results:
If your doctor suspects bile duct cancer, an abnormal CA 19-9 blood level will increase the suspicion. However, there are benign diseases of the bile ducts and pancreas that occasionally result in elevated CA 19-9 levels. For this reason CA 19-9 is not considered a diagnostic test.
Pathology Tests ▼
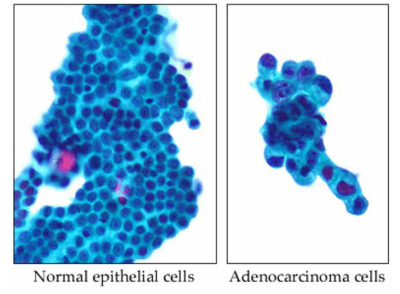
Pathology is the gold standard for the diagnosis of cancer. The diagnosis can sometimes be made by cytopathology, the study of individual cells spread into a thin layer onto glass microscopic slides.
1. Fine Needle Aspiration (FNA)
Bile duct brushings can be performed through an endoscope (a special scope which is inserted into the mouth and passed into the first portion of the intestine) to detect malignant cells. If a mass is present, fine needle aspiration of it can be performed; this involves guiding a thin needle into the lesion, and gently sucking out cells for microscopic examination. These procedures have the benefit of not requiring an operation or general anesthesia.
A method to biopsy, obtain cells, for examination under the microsope.
FNA, performed in conjunction with a CT or MRI imaging, enables pathologists to determine the nature of a suspicious biliary tract abnormality.
Procedure:
It is a surprisingly safe procedure that involves passing a small needle directly through the skin or through an endoscope. The CT or MRI imaging allows the doctor to see where the needle is going. This is because the needle used has a very small bore. This sometimes means that the small amount of tissue obtained is insufficient for the pathologist to establish a diagnosis.
Accuracy:
A diagnosis of biliary cancer based on a FNA is highly accurate, approaching 99%. However, it is only between 50-70% accurate in determining whether the cancer is benign or malignant.
Because the amount of tissue obtained is so small, the absence of malignant cells in the sample cannot exclude the possibility of malignant disease altogether.
Risks:
Complications such as bleeding or infection occur very rarely, less than 1% of patients.
Note:
Another technique used to obtain cells from the biliary tree for examination is bile duct brushing. In this procedure, through an endoscope, a brush is used to remove cells from the inside of the bile duct. These cells are smeared onto a slide and examined under the microscope.
2. Biopsy
Biopsy of the biliary tract is the more common means of detecting these tumors. Sometimes the biopsies can be performed through the endoscope; other times exploratory laparotomy, in which the surgeon makes an incision in the abdominal wall and enters the abdomen, is performed, under general anesthesia.

