Type 1 Diabetes
What is Type 1 Diabetes?
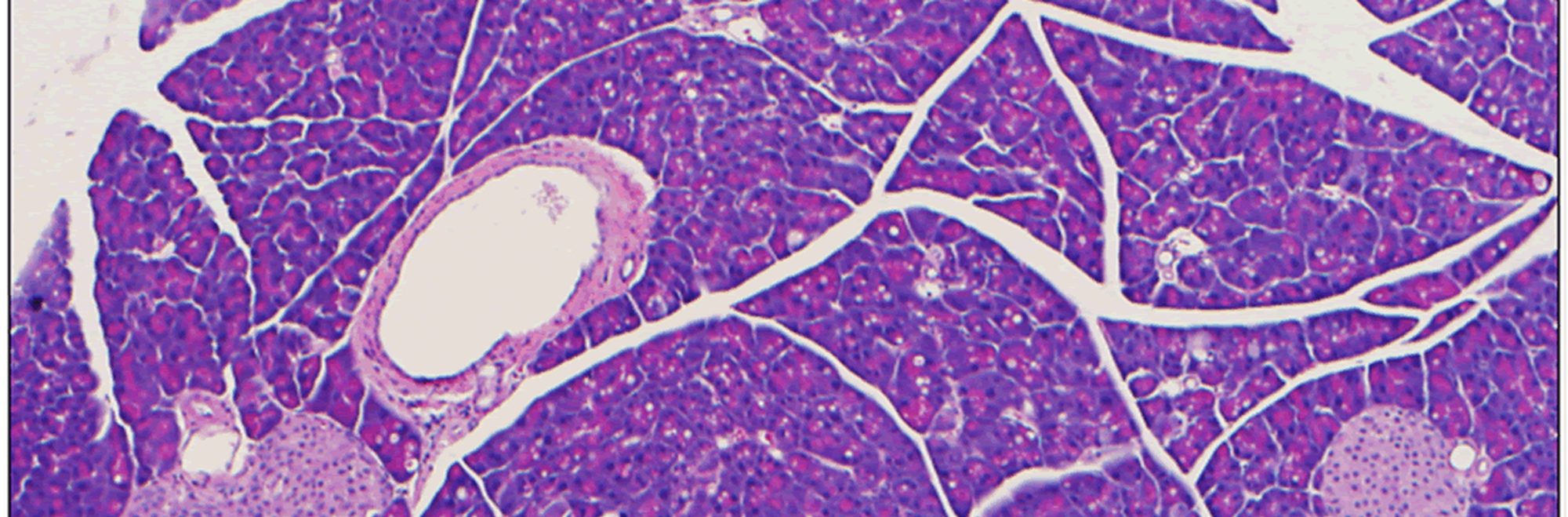
Type 1 Diabetes, also called autoimmune diabetes, results from mistaken recognition of islets of Langerhans, the only source of insulin in the body, as a foreign entity by the individual's own immune system. As a consequence, different cell types of the immune system led by T cells work together to invade the pancreas and destroy pancreatic islets, leading eventually to their destruction and insulin deficiency.
Current Treatments
Before the discovery of insulin almost 100 years ago, Type 1 Diabetes was invariably fatal due to hyperglycemia (high blood sugars) and ketosis. Insulin therapy has therefore been a lifesaver for Type 1 Diabetes patients. However, insulin replacement is not a cure and needs to be used on regular basis and on demand as advised by physicians.
While life sustaining, insulin therapy is complicated and can cause hypoglycemia (low blood sugar levels), which can be dangerous and even life threatening. Therefore, it is important for patients to constantly monitor their blood sugar levels, carefully watch their diets, and follow personalized regimens to avoid clinically significant excursions of hypoglycemia and hyperglycemia, and long term complications.
Research: Looking Ahead
Following the recommended insulin regimens is not easy, especially among young diabetic patients and kids. Only about 1/3 of Americans with Type 1 Diabetes are consistently achieving recommended blood glucose levels.
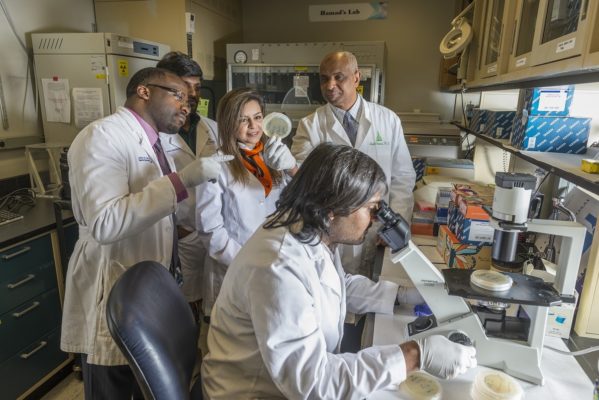
Because of the constraints of insulin therapy, scientists around the globe— including our own group here at Johns Hopkins— have been working around the clock to understand the disease pathogenesis (development) and develop strategies to prevent or arrest the disease at or before onset.