Major research efforts focus on the neurobiology/neuropathology and pathogenic mechanisms involved in a variety of illnesses, including neurodegenerative diseases (amyotrophic lateral sclerosis, Alzheimer's disease, Huntington's disease, and Parkinson's disease), pediatric and adult brain tumors, and peripheral nerve disease. We also research neoplastic and non-neoplastic diseases of the eye. Our researchers use a variety of in vitro and in vivo experimental systems, including human tissues and animal models of neurodegenerative diseases and cancer.
Alzheimer's Disease
Alzheimer's disease (AD) is the most common form of neurodegenerative disorder occurring in mid to late life. Among the individuals 65 years of age or older, 7-10% of the population is affected by AD. Because of significant increase in life expectancy, the prevalence of AD will increase dramatically worldwide. It is estimated that the incidence of AD will increase by over 100% in the industrial countries, and by more than 300% in developing countries, which makes the understanding of AD a central topic of medical research worldwide.
Please check the Alzheimer's Disease Research Center site.
Current Research
- Juan Troncoso, M.D.
Network Dynamics of Amyloid Beta Protein in Postmortem Specimens from Subjects 30 to 65
- Juan Troncoso, M.D.
High Field Imaging of Postmortem Brains
- Philip Wong, Ph.D.
Developing New Animal Models for AD
Amyotrophic Lateral Sclerosis
coming soon...
Huntington's Disease
Huntington's disease (HD) is a progressive, fatal, neurodegenerative disorder inherited as an autosomal dominant trait. HD is caused by an expanded CAG repeat in the huntingtin (HTT) gene, located in the short arm of chromosome 4, which encodes an abnormally long polyglutamine repeat in the huntingtin protein (HD Collaborative Group 1993). Prevalence of Huntington's disease is 4-10 per 100,000 in the western world, with many more people at risk of the disease. Mean age of onset is 40 years, with death occurring 15-20 years from onset. Clinical features of Huntington's disease include progressive motor dysfunction, cognitive decline, and psychiatric disturbance (Ross et al. 2001; Walker 2007; Ross et al. 1997). The pathological hallmark of HD is the degeneration and atrophy of the striatum, but as the disease progresses there is also involvement of the cerebral cortex and other subcortical structures. Although the mutation that causes HD was discovered almost 20 years ago, we still do not understand the mechanism by which the abnormally long polyglutamine repeat in the HTT protein causes the degeneration of nerve cells in specific brain regions. This is particularly puzzling since HTT is expressed in all brain regions. Nevertheless, understanding the genetics of HD has helped investigators to develop animal and cellular models to examine the pathogenesis of the disease. These models have led to the notion that mutated HTT is toxic to striatal neurons and that this toxicity is probably related to one or a few of the more than hundred proteins that interact with HTT (Ross and Tabrizi 2011; Subramaniam et al. 2011). As valuable as they are, animal and cell models of HD (Schilling et al. 2007; Ratovitski et al. 2011) are not enough on themselves to unravel the pathogenesis of HD and discover an effective treatment. The hypotheses developed by using these models need to be validated by examining and testing human autopsy tissues from HD patients and also control subjects. Thus, a very important and critical role of autopsy in HD cases is to provide postmortem tissues for research purposes. This is the function of the Neuropathology Core of the Johns Hopkins University Huntington's Disease Research Center without Walls and the Brain Resource Center (BRC).
Clinical features and diagnosis of HD
The clinical manifestations of HD usually present between the ages of 35 and 45 years, but can begin at any age from childhood to old age. The motor features of HD are pleomorphic; in some cases chorea is the dominant feature, while in others there is more prominent motor impairment manifest by rigidity, bradykinesia, and incoordination. Chorea are involuntary and uncontrollable jerky movements of extremities and facial muscles. Cognitive impairment in HD is initially subtle and affects predominantly executive functions, but there is also eventually impairment of various types of memory. These cognitive impairments are progressive and many patients develop a full dementia. HD patients also present behavioral abnormalities including anxiety, depression, and compulsive behaviors. The diagnosis of HD is based on the clinical history, neurologic and psychiatric examinations, neuroimaging, and the genetic test that counts the number of CAG repeats in each of the two HTT alleles.
The disease is inherited in an autosomal dominant manner with age-dependent penetrance, and repeat CAG lengths of 40 or more are associated with nearly full penetrance by age 65 years (International Huntington's Disease Collaborative Group 2004) individuals at risk of inheriting the expanded CAG nucleotide can be identified before clinical onset by predictive genetic testing. Longer CAG repeats predict earlier onset, accounting for up to 50-70% of variance in age of onset, with the remainder likely to be due to modifying genes and the environment (Wexler 2004).
Neuropathologic features and postmortem diagnosis of HD
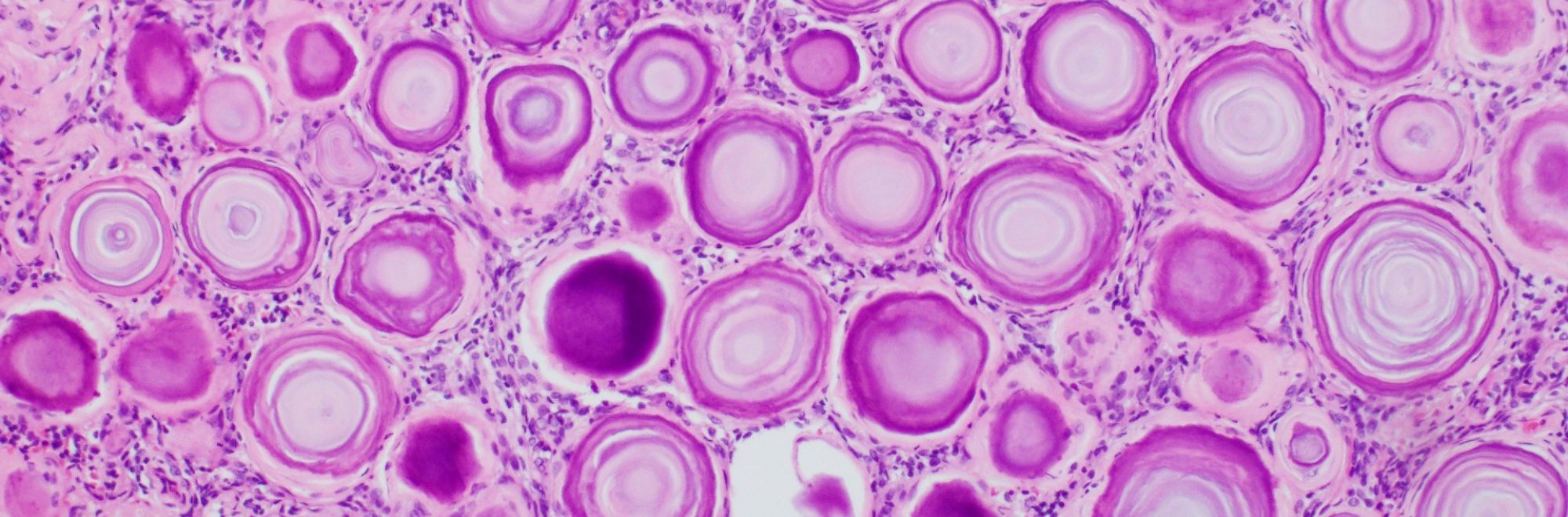
Gross examination of the brains in the very early stages of HD may show minimal or no changes, but in advanced cases it generally shows diffuse atrophy and low weight. In our experience, the average postmortem brain weight in HD is 1097 gm with a range from 600 gm to 1368 gm (normal average is 1400 gm). External examination shows frontal and parietal gyral atrophy in ~80% of the cases and atrophy of the striatum in ~95% (Vonsattel et al. 1998). Quantitative studies have shown reductions in cross-sectional areas in various anatomical compartments: eg 21-29% in cerebral cortex, 28% in thalamus, 57% in the caudate, and 64% in the putamen in moderately affected cases (de la Monte et al. 1988). Microscopic changes in HD are most severe in the striatum, where neuronal loss is accompanied by striking astrocytosis. In the striatum, the medium spiny neurons are selectively vulnerable to HD, compared to aspiny neurons (Graveland et al. 1985). Among spiny neurons, those containing enkephalin are more vulnerable than those containing substance P (Reiner et al. 1988).
This selective vulnerability is more obvious in the early stages of the disease, since in end-stage cases, both spiny and aspiny neurons degenerate. Another important pathological feature of HD is the gradient of changes within the striatum. The degeneration of neurons in the caudate progresses from the tail to the body to the head, and it also has a dorsomedial to ventrolateral vector. In the putamen, the loss of neurons advances from caudal to rostral and from dorsal to ventral. The nucleus accumbens is relatively spared (Vonsattel et al. 1998). According to Vonsattel, the severity of pathology of HD autopsy brains can be rated in a 0 to 4 grade system.
This is a practical and now conventional approach to assess the severity of pathology in HD autopsy brains (Vonsattel et al. 1985). The neuronal degeneration of the cerebral cortex in HD becomes evident in advanced stages of the disease (i.e., Vonsattel Grades 3 & 4). Degenerative changes in HD also extend beyond the cerebral cortex and striatum, although to a lesser degree. Antibodies against huntingtin allow for the identification of intranuclear, perikaryal, and neuritic HTT inclusions in HD. Intranuclear aggregates or inclusions of N-terminal fragments of mutated huntingtin were first reported in HD brain (DiFiglia et al. 1997; Becher at al. 1998). The presence of these inclusions is helpful to confirm the diagnosis of HD. Neuropil aggregates of HTT in the brains of HD can be striking and are also detected by immunostains with HTT antibodies.
The autopsy of HD patients is also important to examine for co-morbidities. Since many HD patients die at advanced age, it is important to examine for other common cause of dementia such as Alzheimer's, Parkinson's and Lewy body disease, frontotemporal degeneration, and cerebrovascular disease.
Huntington's Disease Research and Tissue Bank at Johns Hopkins
The Research Center without Walls for Huntington's Disease at the Johns Hopkins School of Medicine, a program supported by NINDS (NS16375), is the hub for HD research at our institution. This Center has an autopsy program based in the Division of Neuropathology which includes a Huntington's disease brain bank. Members of the HD research community at Hopkins and other institutions are welcome to apply for postmortem tissue samples. Even though much is known about HD, many important features of the disease are still poorly understood. Research on human HD brain tissue is still critical for understanding the biology of the disease and for developing new treatments. Current research includes studying Htt and its interacting proteins using modern quantitative proteomic techniques, and using modern techniques of molecular biology to understand gene expression changes in HD. These studies will be critical for developing novel treatments for the disorder. To this end, please contact Dr. J. Troncoso ([email protected]) or Dr. Christopher Ross ([email protected]).
REFERENCES
- Becher, M, Kotzu J, et al. (1998). "Intranuclear neuronal inclusions in Huntington's disease and dentatorubral and pallidoluysian atrophy: Correlation between the density of inclusions and IT15 CAG triplet repeat length." Neurobiol Dis 4:387-397.
- de la Monte SM, Vonsattel JP, et al. (1988). "Morphometric demonstration of atrophic changes in the cerebral cortex, white matter, and neostriatum in Huntington's disease." J Neuropathol Exp Neurol 47(5):516-25.
- DiFiglia, M., Sapp E, et al. (1997). "Aggregation of huntingtin in neuronal intranuclear inclusions and dystrophic neurites in brain." Science 277(5334):1990-3.
- Graveland GA, Williams RS, et al. (1985). "Evidence for degenerative and regenerative changes in neostriatal spiny neurons in Huntington's disease." Science 227(4688):770-3.
- HD Collaborative Group. (1993). "A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington's disease chromosomes." Cell 72(6):971-983.
- International Huntington's Disease Collaborative Group, Langbehn DR, Brinkman RR, Falush D, Paulsen JS, Hayden MR. (2004). "A new model for prediction of the age of onset and penetrance for Huntington's disease based on CAG length." Clin Genet 65:267-277.
- Ratovitski T, Chighladze E, Waldron E, Hirschhorn RR, Ross CA. (2011). "Cysteine proteases bleomycin hydrolase and cathepsin Z mediate N-terminal proteolysis and toxicity of mutant huntingtin." J Biol Chem. 286(14):12578-89.
- Reiner A, Albin RL, et al. (1988). "Differential loss of striatal projection neurons in Huntington disease." Proc Natl Acad Sci U S A 85(15):5733-7.
- Ross CA, Margolis RL, Rosenblatt A, Ranen NG, Becher MW, Aylward E. (1997). "Huntington disease and the related disorder, dentatorubral-pallidoluysian atrophy (DRPLA)." Medicine (Baltimore) 76:305-338.
- Ross CA, Tabrizi SJ. (2011). "Huntington's disease: from molecular pathogenesis to clinical treatment (Review)." The Lancet Neurology 10(1):83-98.
- Schilling G, Savonenko AV, Klevytska A, Morton JL, Tucker SM, Poirier M, Gale A, Chan N, Gonzales V, Slunt HH, Coonfield ML, Jenkins NA, Copeland NG, Ross CA, Borchelt DR. (2007). "Nuclear-targeting of mutant huntingtin fragments produces Huntington's disease-like phenotypes in transgenic mice." J Neuropathol Exp Neurol. 66(4):313-20.
- Subramaniam S, Snyder SH. (2011). "Huntington's disease is a disorder of the corpus striatum: focus on Rhes (Ras homologue enriched in the striatum)." Neuropharmacology 60:1187-92. Vonsattel JP, Myers RH, et al. (1985). "Neuropathological classification of Huntington's disease." J Neuropathol Exp Neurol 44(6):559-77.
- Vonsattel JP, DiFiglia M (1998). "Huntington disease." J Neuropathol Exp Neurol 57(5): 369-84.
- Walker FO. (2007). "Huntington's disease." Lancet 369;218-228.
- Wexler NS. (2004). "Venezuelan kindreds reveal that genetic and environmental factors modulate Huntington's disease age of onset." Proc Natl Acad Sci USA 101:3498-3503.
Parkinson's Disease
coming soon...
Stroke and Brain Ischemia
coming soon...
Brain Injury and Degeneration
Visit our Brain Injury and Degeneration
We also offer an ACGME-accredited training program leading to eligibility for Board certification in Neuropathology.