Diagnostic Tests
Pancreatic cancer often presents clinically with non-specific signs and symptoms such as pain, jaundice (yellowing of the skin) and weight loss. In these situations the diagnosis of pancreatic cancer may not be suspected and even when pancreatic cancer is suspected, the cancer can be difficult to detect and even more difficult to diagnose. A variety of techniques can be used to establish a diagnosis.
These techniques include:
Blood tests (such as a CA 19-9) ▼
Physicians usually perform a variety of blood tests on patients suspected of having pancreatic cancer. We would like to emphasize three of them.
CA 19-9
CA19-9 is a tumor marker for pancreas cancer that is measured with a blood test. CA 19-9 levels can assist with an initial diagnosis, as the levels of this marker can be elevated in people with pancreatic cancer. In pancreatic cancer patients with elevated CA 19-9 levels, the levels of this marker can be used to measure the response of the cancer to treatment. In general, a declining or stable CA19-9 levels generally indicates that the tumor is responding to treatment, while increasing levels indicate the progression of disease. The old adage, "treat the patient not blood numbers," should be remembered. If a patient is feeling better and the tumor shrinks, that is what matters. Of note, cells in some patients cannot make CA19-9, and CA 19-9 levels are of no use in these patients.
Blood glucose level
Pancreatic cancer is associated with abnormalities in blood glucose (sugar) levels. Long-standing diabetes mellitus (sugar diabetes) is a risk factor for developing pancreatic cancer, and new onset diabetes in a person above the age of 50 years can be an early sign of pancreatic cancer. Patients with diabetes often have abnormally high blood glucose levels. Doctors may therefore draw blood from the patient's arm in order to measure their blood glucose levels. Abnormally high levels may suggest diabetes. Abnormally low levels can be seen in a variety of conditions, including the very rare neuroendocrine tumor of the pancreas called a "glucagonoma."
Blood bilirubin level
As discussed earlier in the anatomy section, the liver produces fluid called bile. Bile made in the liver collects in tubes (the bile ducts) in the liver. These bile ducts join together to form a larger tube called the common bile duct. The common bile duct drains into the duodenum where the bile assists in the digestion of food. At one point along its course, the common bile duct passes through the pancreas. Cancers arising in the pancreas can impinge upon the bile duct and block the flow of bile. This blockage of the flow of bile may produce a yellowing of the white portion of the eyes (called jaundice), and in some patients jaundice is the first presentation of their pancreatic cancer. Doctors may therefore draw blood from the patient to test it for "bilirubin" levels (one of the components of bile). High bilirubin levels, called hyperbilirubinemia, would suggest that there is something obstructing the normal flow of bile such as a tumor in the pancreas.
Radiology (CT, MRI, PET) ▼
Radiographic imaging is in many ways the mainstay of managing patients with pancreatic cancer. A number of technologies can be used to visualize pancreatic masses, but we would like to emphasize the four most common- computerized axial tomography (CAT) scanning, endoscopic ultrasound (EUS), positron emission tomography (PET), and magnetic resonance imagining (MRI).
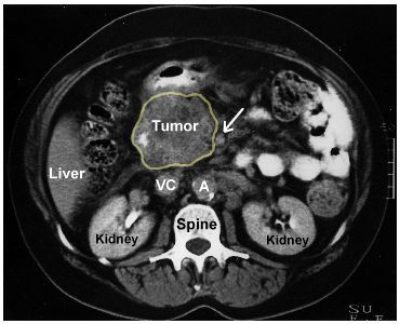
CT Scan (computerized axial tomography)
CT scans are generated using a special machine (of course called a CAT scanner!) that rapidly directs multiple X-ray beams from multiple different angles and levels to the abdomen. Contrast dye, given to the patient by mouth (orally) and/or into the blood stream (intravenously), can help make the organs visible by appearing white on the X-ray films. A computer processes the X-ray information and produces the CT images, usually as cross-sectional slices of the abdomen. Exquisitely detailed three-dimensional images can now also be produced using advanced image processing methods. CT scans can now be performed in 20-30 seconds using newer machines.
CT scanning will visualize the vast majority of pancreatic cancers, and it provides important information to guide treatment. For example, the relationship of the cancer in the pancreas to important blood vessels adjacent to the pancreas can be seen, a feature used by surgeons to determine if the tumor can be safely removed surgically. The liver and other organs are also visualized, helping to determine if the cancer has spread ("metastasized") beyond the pancreas.
The level of radiation received during a CT scan is modest. Apart from the minute risk (much less than 1% of patients) of an allergic reaction to the contrast dye, a CT scan is without major complication. It is always advisable to inform your doctor of any allergies you have.
CT scans are often the first test doctors order when they suspect a pancreatic cancer, because it is considered one of the most useful imaging techniques.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is often used to image the pancreas because it doesn’t use X-rays (ionizing radiation). Instead, a series of powerful magnets and specialized detectors are used to create an accurate image of the pancreas and surrounding structures. The detail seen (resolution) of MRI isn't as good as it is with endoscopic ultrasound (EUS) and CT scanning, but MRI can provide detailed images of the pancreatic duct system (a procedure sometimes referred to as "MRCP").
Positron Emission Tomography
Radioactively labeled sugars (18F-fluorodeoxyglucose [FDG]) are given to the patient and the radioactive tracer is concentrated in areas of the body that actively metabolize (use) sugar. Since many cancers actively metabolize sugar, positron emission tomography (PET) scanning is an excellent technology to evaluate the activity of a tumor.
For example, if a patient has been treated for pancreatic cancer and CT scanning reveals that a lesion remains where the cancer was, PET scanning can be used to determine if the remaining lesion is a scar or if it is actively growing tumor. Scar tissue would be negative on PET scan, while active tumors are often PET positive ("PET avid"). PET scanning is sometimes combined with CT scanning, a test called PET/CT.
Endoscopic Ultrasound (EUS) and Endoscopic Retrograde Cholangiopancreatography (ERCP) ▼

Endoscopic ultrasound (EUS) is a significant improvement over the standard (transabdominal) ultrasound. During standard transabdominal ultrasound the ultrasound probe is placed externally on the surface of the abdomen which limits the resolution of the images. EUS is an improvement on this technique because the ultrasound probe is placed much closer to the pancreas. The ultrasound probe is placed in close proximity to the pancreas by attaching it to the end of a standard gastrointestinal endoscope and passing the endoscope in the mouth, down the esophagus and into the stomach and duodenum. The close proximity of the ultrasound probe to the pancreas produces very detailed images.
EUS enables the doctor, called an endoscopist, to identify small (<1 centimeter; <1/2 inch) abnormalities in the pancreas. There are small pancreas cancers that can be detected with EUS that cannot be visualized currently with a CT scan. Technological improvements are enabling a generation of even more accurate EUS images of the pancreas and such improvements are expected to continue.
Although EUS can visualize small masses it cannot be used to make a diagnosis of cancer with certainty. For this reason, EUS is often combined with a biopsy. One advantage of the EUS procedure is that this biopsy can be taken through the EUS endoscope.
The main variable in the success of an EUS investigation is the experience of the endoscopist. The technique is difficult and the optimal use of this technique depends on the considerable skill of the endoscopist.
Biopsy Interpreted by a Pathologist ▼
Cancer is just one of many processes that can produce a mass lesion in the pancreas. Some forms of inflammation of the pancreas produce masses (such as autoimmune pancreatitis) as do some benign (non-cancerous) tumors. A mass detected in the pancreas by imagining techniques therefore is not necessarily a cancer. The "gold standard" for diagnosing pancreatic cancer remains the biopsy (sampling of a small amount of tissue from the mass followed by examination of the tissue sampled using a microscope). Imagining is therefore usually followed up with a biopsy. Biopsy can take a number of forms including fine needle aspiration (FNA), tissue needle core biopsy, or by excisional biopsy at the time of surgery.
Fine needle aspiration (FNA) samples can be obtained through the EUS endoscope, or in conjunction with a CAT or MRI imaging. It is a safe procedure that involves passing a thin needle directly through the EUS endoscope or through the skin and into the tumor. The diagnosis of a pancreatic cancer based on a fine needle aspiration (FNA) is highly accurate, approaching 99%. However, in some instances, because the amount of tissue obtained is so small, a definitive diagnosis cannot be made. In these cases the biopsy procedure may have to be repeated. Biopsies obtained at the time of surgery are usually larger, and more often produce a definitive diagnosis.
Biopsies can be used to both determine if a tumor is present and, if a tumor is present, to classify the type of tumor. Pathologists are doctors specially trained to interpret these biopsies. Pathologists look at tissue from a biopsy (a small sample of tissue) as well as tissue from a resection (portions of organs or entire organs removed during surgery). The tissue is examined under a microscope to determine whether or not it is cancer and what kind of cancer it is. Typically, patients will not meet the pathologist interpreting their tissue. Like radiologists, the findings of the pathologist will be given in a report available to the other physicians on your team.
Screening and Early Detection ▼
Hope Through Early Detection
Johns Hopkins’ world-renowned experts, Dr. Anne Marie Lennon and Dr. Marcia Canto, discuss the early detection of pancreatic cancer to talk about cutting-edge diagnostics that will create a different future for those most at risk for pancreatic cancer.
Screening Asymptomatic Patients
Although there are no screening tests currently available to screen the general population, investigators at Johns Hopkins are working on developing new tests such as the endoscopic ultrasound. It is hoped that these new tests may prove effective, particularly when applied to slect groups of patients known to have an increased risk of developing pancreatic cancer such as individuals with a strong family history of pancreatic cancer.
CA19-9 is the best available tumor marker for following the progression of the disease but is only 80% accurate in identifying patients with pancreatic cancer. Due to the inability of CA19-9 to identify early potentially curable disease, several other markers have been studied including SPAN-1, CA-50, DUPAN-2, elastase-1, tissue polypeptide antigen and tissue polypeptide-specific antigen. These markers have not performed nearly as well as the CA19-9.
An ideal pancreatic cancer screening test should be a safe, inexpensive, highly accurate test that reliably diagnoses pancreas cancer at a stage when it is not causing symptoms in the patient. This would provide that person the opportunity to take appropriate and effective action to treat and potentially cure the disease. Currently, we cannot offer a screening test for pancreas cancer that begins to meet these demands. However, the potential for screening this disease is considerably improved compared to just a few years ago.
First of all, we know more about which individuals have a genetic predisposition for developing this disease. Prior to the 1990's, it was not widely appreciated how often pancreas cancer is an inherited disease. Now we know that individuals with abnormalities in certain genes, such as BRCA2, p16, HNPCC, and individuals with histories of familial pancreatitis and Peutz-Jeghers syndrome are all predisposed to pancreatic cancer. These are important discoveries. However, individuals who inherit damage to one of these genes still represent only a modest proportion of all those individuals at risk of developing pancreatic cancer.
Secondly, we now know much more about the changes in the DNA and other molecules in the pancreas cells that give rise to pancreatic cancer. Most of these changes are not inherited and occur as the result of factors such as smoking, diet, and age. Importantly, pancreatic cancer researchers are characterizing these specific changes in DNA and other molecules. Armed with this knowledge, it is hoped that over the next few years, specific and extremely sensitive screening tests will be developed. Such a screening test will be able to detect pancreatic cancer at an early stage when it still cannot be visualized using state of the art diagnostic imaging techniques. Once such a screening panel is in place, it can be offered to individuals who, from their family history, know that they are at particular risk of developing this disease.
Because of the enormous need to develop a sensitive and specific screening text for early pancreatic cancer, we have a research laboratory at Johns Hopkins dedicated to finding new screening tests for pancreatic cancer. This lab is headed by Dr. Michael Goggins.
Visit Pancreatic Cancer Early Detection Lab