Intraductal papillary mucinous neoplasms (IPMNs) are tumors that grow within the pancreatic ducts.
About IPMNs
Intraductal papillary mucinous neoplasms are tumors that grow within the pancreatic ducts (the pancreatic ducts are the "tubes" within the pancreas that are used to transport fluids to the bowel to help with digestion). Intraductal papillary mucinous neoplasms are also characterized by the production of thick fluid, or "mucin", by the tumor cells.
IPMNs are important because some of them progress to invasive cancer if they are left untreated. Just as colon polyps can develop into colon cancer if left untreated, some IPMNs can progress into invasive pancreatic cancer. IPMNs therefore represent an opportunity to treat a pancreatic tumor before it develops into an aggressive, hard-to-treat invasive cancer.
On the other hand, most IPMNs will never progress to a cancer, and it can be safe to observe (rather than treat) those IPMNs that don't progress. The challenge for clinicians is to determine which IPMNs need to be removed surgically and which IPMNs can be safely observed.
For a comprehensive discussion of pancreatic cysts and IPMNs, watch the webcast by Dr. Anne Marie Lennon.
IPMN FAQs
The management of IPMNs can be complicated, so we provide answers to common questions our patients have about IPMNs. We hope you find this information helpful.
How common are IPMNs? ▼
Intraductal papillary mucinous neoplasms are surprisingly common. We completed a study here at Johns Hopkins Hospital in which we carefully studied the pancreatic findings in a large series of patients who underwent computerized tomography (CT) scanning that included their pancreas.
We found that 2.6 out of every 100 healthy individuals examined had a pancreatic cyst (IPMN). There was a strong correlation between pancreatic cysts and age. No cysts were identified among asymptomatic individuals less than 40 years of age, while 8.7 percent of the patients age 80 to 89 years had a pancreatic cyst. Thus, intraductal papillary mucinous neoplasms of the pancreas are fairly common, particularly in the elderly.
What do IPMNs look like under a microscope? ▼
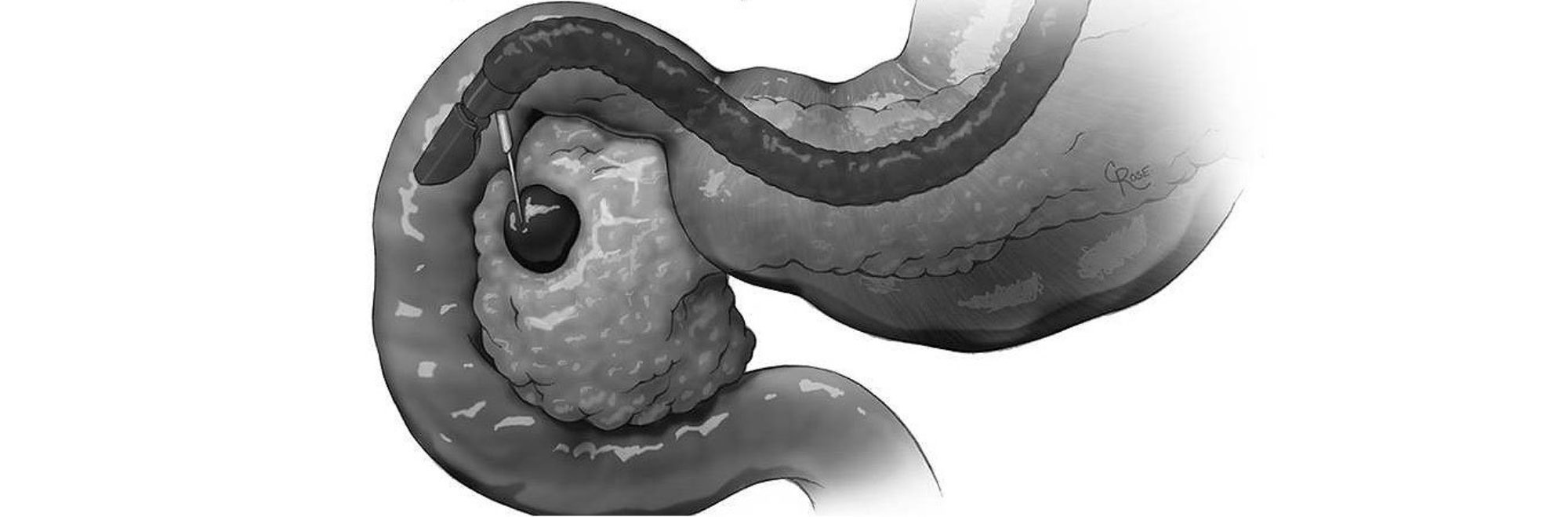
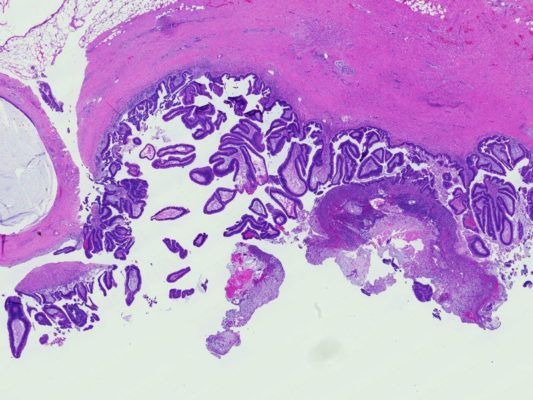
The main pancreatic duct is the long branching tube-like structure that runs down the center of the pancreas. It collects the digestive enzymes made by the pancreas from branch ducts that run into it like a stream into a river, and delivers the digestive enzymes to the intestine (duodenum). Intraductal papillary mucinous neoplasms (IPMNs) arise within one of these pancreatic ducts. Grossly (using the naked eye), intraductal papillary mucinous neoplasms (IPMNs) form tumors that project into the duct (click here to compare IPMNs with other cysts). When examined using a microscope, intraductal papillary mucinous neoplasms can be seen to be composed of tall (columnar) tumor cells that make lots of mucin (thick fluid).
Pathologists classify intraductal papillary mucinous neoplasms (IPMNs) into two broad groups - those that are associated with an invasive cancer and those that are not associated with an invasive cancer. This separation has critical prognostic significance. Patients with a surgically resected intraductal papillary mucinous neoplasm without an associated invasive cancer have an excellent prognosis (>95% will be cured), while patients with a surgically resected intraductal papillary mucinous neoplasm with an associated invasive cancer have a worse prognosis.
Intraductal papillary mucinous neoplasms without an associated invasive cancer can be further subcategorized into two groups. They are IPMN with low-grade dysplasia, and IPMN with high-grade dysplasia. This categorization is less important than the separation of IPMNs with an associated cancer from IPMNs without an associated invasive cancer, but this categorization is useful as IPMNs are believed to progress from low-grade dysplasia to high-grade dysplasia to an IPMN with an associated invasive cancer.
What is the difference between main duct and branch duct IPMNs? ▼
Intraductal papillary mucinous neoplasms (IPMNs) form in the main pancreatic duct or in one of the branches off of the main pancreatic duct.
IPMNs that arise in the main pancreatic duct are called, as one might expect, "main duct type" IPMNs. Think of a tumor involving the trunk of a tree. IPMNs that arise in one of the branches of the main duct are called "branch duct type" IPMNs. Think of a tumor involving a branch of a tree.
The distinction between main duct type and branch duct type IPMNs is important because several studies have shown that, for each given size, main duct IPMNs are more aggressive than are branch duct IPMNs and branch duct IPMNs are less likely to give rise to an invasive cancer. For this reason, most main duct IPMNs are surgically resected, while some branch duct IPMNs can be safely observed.
What symptoms do IPMNs cause? ▼
Signs and symptoms include:
- abdominal pain
- nausea
- vomiting
- jaundice (a yellowing of the skin and eyes caused by obstruction of the bile duct)
- weight loss
- acute pancreatitis
These signs and symptoms are not specific for an IPMN, making it difficult to establish a diagnosis. Doctors will often order additional tests.
A growing number of patients are now being diagnosed by chance, before they develop symptoms (asymptomatic patients). In these cases, the lesion in the pancreas is discovered accidentally when the patient is being scanned for another reason. For example, we have seen patients who had a CAT scan because they were in a car accident; the CAT scan happened to include the pancreas and it revealed an unsuspected IPMN.
How are IPMNs diagnosed? ▼

If a doctor has reason to believe that a patient may have an IPMN, he or she can confirm that suspicion using one of a number of imaging techniques, including computerized tomography (CAT or CT scan), endoscopic ultrasound (EUS), and magnetic resonance cholangiopancreatography (MRCP). These tests will reveal enlargement (dilatation) of the pancreatic duct or one of the branches of the pancreatic duct.
In some cases a fine needle aspiration (FNA) biopsy can be obtained to confirm the diagnosis. Fine needle aspiration biopsy is most commonly performed through an endoscope at the time of endoscopic ultrasound.
How are main duct type IPMNs treated? ▼
As many as 70% of main duct type intraductal papillary mucinous neoplasms harbor high-grade dysplasia (the step right before an invasive cancer develops) or an invasive cancer. Main duct type IPMNs are therefore clinically high-risk lesions, and, in general, most main duct intraductal papillary mucinous neoplasms should be surgically resected if the patient can safely tolerate surgery. It is important that this surgery is carried out by surgeons with ample experience with pancreatic surgery.
IPMNs in the tail of the pancreas are usually resected using a procedure called a "distal pancreatectomy." Surgeons at Johns Hopkins perform some distal pancreatectomies using minimally invasive procedures (laproscopic pancreatectomy). IPMNs in the head or uncinate process of the pancreas are usually resected using a Whipple procedure (pancreaticoduodenectomy). A total pancreatectomy (removal of the entire gland) may be indicated in the rare instances in which the intraductal papillary mucinous neoplasm involves the entire length of the pancreas.
Read More about Treatment TypesHow are branch duct type IPMNs treated? ▼
The management of branch duct IPMNs is more complicated than is the management of main duct type IPMNs. Many branch duct IPMNs are harmless and the risks associated with surgery may outweigh the benefits of resecting them.
If you have a branch duct IPMN, you should consult with a physician to determine the the most suitable methodology to follow your IPMN as well as the frequency of follow-up.
International consensus guidelines for the treatment of branch duct IPMNs were updated in 2017. These guidelines balance the risks and benefits of treating patients with a branch duct type IPMN. The guidelines suggest that asymptomatic patients with a branch duct IPMN that a) is less than 3 cm in size, b) not associated with dilatation (ballooning) of the main pancreatic duct, and c) does not contain a solid mass (mural nodule), can be followed safely without surgery.
By contrast, the guidelines recommend the surgical resection of branch duct type IPMNs that cause symptoms, that are larger than 3 cm, that contain a mass (mural nodule), OR which are associated with significant dilatation of the main pancreatic duct. These guidelines have been supported by a number of recent studies. The rate of growth of an IPMN and preferences of the patient and surgeon also guide the management of IPMNs. Unfortunately, the criteria used to guide the clinical management of a patient with an IPMN are not perfect. Some IPMNs that meet criteria for surgery, when removed, will prove to be of the harmless type (they have low-grade dysplasia). Branch duct IPMNs should be surgically resected only if the patient can safely tolerate surgery. Branch duct IPMNs that are not surgically resected can be monitored clinically to make sure that they do not grow. Growth of a branch duct IPMN or the development of a mass (mural nodule) while being monitored may be an indication to surgically remove the IPMN.
Several imaging technologies can be used to monitor branch duct IPMNs for growth. These include computerized tomography (CT), endoscopic ultrasound (EUS), and magnetic resonance cholangiopancreatography (MRCP). In general, smaller branch duct IPMNs less than 1 cm in size can be followed with an annual exam. Patients with larger IPMNs may have an examination more frequently, some as frequently as every three months.
If I had an IPMN surgically removed, am I cured? ▼
While patients who undergo resection of an IPMN not associated with an invasive cancer are "cured" of that particular lesion, IPMNs can be multiple and patients with one IPMN remain at risk for developing a second lesion in the part of the pancreas that wasn't removed.
Therefore, your doctor will recommend follow-up visits after surgery for an IPMN.
Am I at increased risk of developing tumors outside my pancreas? ▼
Patients with an IPMN have been shown to have a slightly increased risk of developing tumors of the colon and rectum. Your doctor may therefore recommend periodic follow-up examination of your colon (via colonoscopy).
How can I be evaluated and treated at Johns Hopkins for an IPMN? ▼
If you have an IPMN and would like to consult with a physician at Johns Hopkins we recommend that you contact our cyst clinic. It is extremely important that you choose a team of specialists with the most up to date knowledge, broad experience, and compassion.
We pledge to take great care of you.
More about the Cyst ClinicEndoscopic Ultrasound FAQs
Endoscopic ultrasound (EUS) is a minimally invasive endoscopic technique which allows the doctor (endoscopist) to obtain detailed images of the pancreas. EUS provides the endoscopist with more information than that obtained with CT or MRI imaging. EUS can be used to evaluate solid masses and to evaluate cystic masses of the pancreas. Since EUS is often used to evaluate IPMNs, we have included information on the EUS procedure here.
Biopsies from abnormal areas of the pancreas can be taken through the endoscope, avoiding exploratory surgery. In particular, at the time of EUS the endoscopist can use a needle passed through the scope to take sample fluid from a pancreatic cyst. If you have additional questions about your EUS procedure, do not hesitate to contact the doctor performing the procedure.
How is an Endoscopic Ultrasound (EUS) performed? ▼
Watch how an EUS is performed
A thin, flexible tube (endoscope) is passed through the mouth and into the stomach and duodenum. The tip of the endoscope contains a built in miniature ultrasound probe which emits sound waves. These sound waves pass through the lining of the stomach and duodenum creating a visual image of the pancreas and surrounding tissue.
EUS can be used to obtain a needle biopsy of the pancreas or to sample fluid in a pancreatic cyst. This is done by passing a very thin needle from the endoscope into the pancreas under continuous ultrasound monitoring. This technique is called EUS-fine needle aspiration (EUS-FNA) and does not hurt.
Another, similar video, showing how EUS is performed with fine needle aspiration
Where is an EUS performed? ▼
EUS is performed as an outpatient procedure (the patient is not admitted to the hospital). Procedures are performed either in the morning or afternoon. As you will be receiving intravenous (IV) sedation you will not be allowed to drive after the procedure. It is important that you have a companion (family member or friend) to take you home and plan to have someone stay with you at home after the examination as sedatives can affect your judgement and reflexes for up to twenty four hours.
Can I eat before the procedure? ▼
EUS procedures are performed either in the morning or afternoon. Make sure you follow the directions you were given about eating and drinking before your procedure. Often, if your procedure is schedule before 12 pm, you will be asked not to eat or drink anything after midnight. Often, if your procedure is scheduled after 12 pm you may allowed to have clear liquids until 8 am on the day of the test. Again, triple check before eating or drinking!
Should I take my medications on the day of an EUS? ▼
If you are taking medication for high blood pressure, seizures, or if you are taking prednisone, you may take these medications the morning of the procedure or at least two hours before the procedure with a sip of water. Do not take any water/fluid pills until after the completion of your procedure.
Anticoagulant medications (blood thinners such as warfarin (Coumadin), heparin, or clopidogrel (Plavix)) may need to be adjusted before the procedure. You should contact your prescribing physician for instruction on when to stop taking this medication. In general aspirin and non-steroidal anti-inflammatory medications (naproxen, ibuprofen etc) can be taken before an EUS examination.
More information, including instructions for patients who are diabetic, is available at Johns Hopkins Gastroenterology and Hepatology. If you have any medical questions about the EUS, please call the nurse coordinator at (410) 502-0793 or the doctor performing the procedure.
How long does the procedure take and what happens afterwards? ▼
The actual EUS procedure usually takes approximately 45-60 minutes. Most patients are discharged 3-4 hours after they arrive. Following the procedure, you will be monitored in the recovery area until the effects of the sedation have worn off. You will be able to eat after the procedure.
Will I be admitted for the procedure? ▼
The procedure is usually performed as an outpatient. Most people are able to go home one to two hours after completion of the procedure.
When will I be given the results of the EUS? ▼
Your endoscopist will usually be able to give you the preliminary results of the EUS on the same day as the procedure. If an EUS-FNA has been performed, these results take between four to five days to return. If you attend the pancreatic cyst clinic, the EUS results will be reviewed along with any other imaging (CT or MRI) and pathology results at the weekly pancreatic cyst multidisciplinary meeting. During this meeting an individualized plan will be developed for you. You will be contacted by a member of the multidisciplinary team within twenty four hours of the meeting to discuss the plan with you.
What are the possible complications associated with EUS? ▼
EUS is a very safe procedure and complications are rare.
You may have a sore throat which usually resolves within a day or two. Sometimes people feel a little bloated due to the air inserted by the instrument.
Other potential but uncommon complications of EUS include a reaction to the sedatives used, aspiration of stomach contents into your lungs, and complications affecting the heart or lungs. One major, but very uncommon complication of EUS is where there is a tear in the lining of the stomach or duodenum, called a perforation, which may require surgery. If an EUS-FNA is performed, where a needle is passed into the pancreas to take a sample, there is a small risk of bleeding, pancreatitis or infection. To decrease the risk of infection, we routinely prescribe antibiotics for patients in whom EUS-FNA was performed on a pancreatic cyst.