The team at Johns Hopkins constantly strives to make research discoveries that will advance the field and improve the outlook for patients in the future. We are not satisfied with the status quo!
The unifying hypothesis that forms the basis for our research at Johns Hopkins is that pancreatic cancer is fundamentally a disease of mutations in cancer-associated genes.
Our efforts began in earnest in 1991 when a surgeon (Charles Yeo) teamed with a pathologist (Ralph Hruban) and a cancer geneticist (Scott Kern). The team obtained a prestigious Specialized Program of Research Excellence (SPORE) grant from the National Institutes of Health in 1993, and we still have this grant in 2020! A real statement of the long-term impact of the science generated by the team at Johns Hopkins. Many talented physician-scientists have joined the team over the years, fostering new careers and productive collaborative pancreatic cancer research.
The Sol Goldman Pancreatic Cancer Research Center was established in 2005, thanks to the generous and visionary philanthropy of the Sol Goldman Charitable Trust, a New York-based philanthropy. This center supports a multi-disciplinary team of physicians and scientists. Since 2005, the center has funded over 150 grants that explore novel areas of research.
Clinical Care ▼
The pancreas cancer team at Hopkins has its origins in patient care. In the 1970s there was no hope for patients with pancreatic cancer. Ninety percent of patients presented with metastatic disease (the cancer had spread to other organs). The only option for patients was surgery, and surgery had a 20-25% operative mortality rate. Dr. John Cameron, then Chairman of Surgery here at Johns Hopkins, dedicated his career to improving pancreatic cancer surgery. In his hands the operative mortality rate fell to less than 2%, and large numbers of patients began to come to Hopkins for treatment. As the team at Hopkins gained more and more experience, the impact of this regionalization of care became dramatic. In the State of Maryland in-hospital mortality rate for pancreatic cancer surgery dropped from 17% to 4.9%. Remarkably, an estimated 61% of this decline was attributable to the increase in share of surgeries performed at Johns Hopkins. For the first time there was a glimmer of hope.
Building on our surgical successes the team created a Pancreas Multidisciplinary Cancer Clinic. This clinic provides patients a comprehensive single day evaluation that incorporates all the resources available for patient education, diagnosis, treatment and research of pancreatic cancer. Faculty from the departments of Oncology, Radiation Oncology, Surgery, Gastroenterology, Pathology, and Radiology participate in the clinic. Patients also meet with clinical trials coordinators. The impact of this team approach to patient care has been dramatic. More than 24% of the patients who have attended the clinic have had a major change to their diagnosis or treatment plan.
While these improvements in clinical care provide hope, they clearly are not enough. More research is needed.
To view the publications list from Sol Goldman Pancreatic Research Center, click the button below.
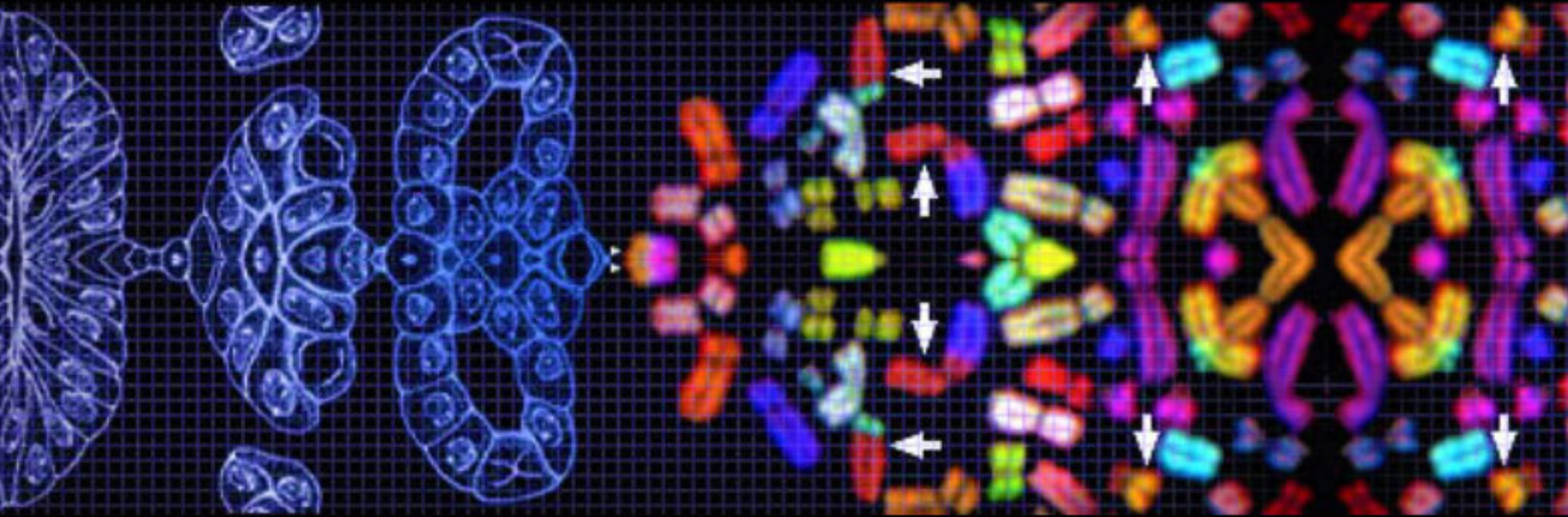
Genetic Profile of Pancreatic Cancer ▼
The pancreatic cancers surgically resected at Johns Hopkins provided a unique opportunity to study the genetics of the disease. Little was known when the team first started studying pancreatic cancer back in 1991.
Led by Scott Kern, the team discovered the SMAD4/DPC4 gene as a driver of pancreatic cancer, and demonstrated that it is mutated in 55% of pancreatic cancers. This discovery launched the field of pancreatic cancer genetics. The team quickly then discovered a genetic change in a pancreatic cancer on chromosome 13q and this discovery, in turn, greatly facilitated the discovery of the breast cancer gene BRCA2. These discoveries represent the fruits of a team approach - surgeons, pathologists, oncologists and molecular biologists working hand in hand using cutting edge technologies to make major discoveries. In 2020, Dr. Ralph Hruban was one of the recipients of the American Association for Cancer Research’s Team Science Award for the National Cancer Research Institute's effort (called the TCGA) to sequence the genes in pancreatic cancer.
As exciting as these discoveries are, they are not enough. The next challenge became to translate them to improved patient care.
The team at Johns Hopkins has characterized the genetic changes in the pancreatic cancer cell lines commonly used by research scientists.
Familial Pancreatic Cancer ▼
The team at Johns Hopkins founded the National Familial Pancreas Tumor Registry (NFPTR) in 1994. To date, over 7,500 families with pancreatic cancer have enrolled in this registry. This national resource is shared with investigators outside of Hopkins, and it has formed the basis for a number of key genetic and epidemiologic discoveries. These include the demonstration that inherited mutations in the BRCA2, STK11, p16/CDKN2A, ATM, PALB2 and hMLH1 genes can cause familial pancreatic cancer. The team has shown that individuals with three or more first-degree relatives with pancreatic cancer have a remarkable 32-fold increased risk of developing pancreatic cancer.
These results have immediate clinical implications. First, based on their family history and genetic status, individuals can be identified who may benefit from screening for early pancreatic neoplasia (see Screening below). Second, the team has shown that pancreatic cancers with BRCA2 gene mutations are exquisitely sensitive to specific therapies ("PARP" inhibitors). Those found to carry a mutation are now treated with specific therapies.
Progression Model ▼
The first step in screening for any cancer is to define the non-invasive precursor lesions that give rise to that cancer. Integrating careful pathologic examination with molecular analyses, the team at Hopkins has characterized the precursors to invasive pancreatic cancer and defined the relative order in which genetic alterations occur in the development of pancreatic neoplasia. Just as colon cancer arises from colon polyps, so too does pancreatic cancer arise from a curable precursor lesion.
The smaller precursor lesions in the pancreas are called "Pancreatic Intraepithelial Neoplasia" (PanIN) and the larger precursor lesions are called "Intraductal Papillary Mucinous Neoplasms" (IPMNs). The team at Hopkins has defined genetic alterations that drive these lesions. Activating point mutations in the KRAS2 gene occur very early in the development of precursor lesions, while p16/CDKN2A is inactivated in intermediate lesions. Inactivating mutations in the SMAD4 and TP53 genes occur in advanced lesions.
These findings are important because genetic changes in early lesions could form the basis of screening tests, while changes in late lesions may be better suited for therapeutic targets.
Early Detection ▼
Much of the team’s effort has focused on developing new approaches to the early detection of curable pancreatic cancers. Two broad approaches have been used.
The first approach has been to find proteins that are made by the cancer cells at levels much higher than normal cells. For example, early on, the team used gene expression platforms including serial analysis of gene expression (SAGE), and "cDNA and oligonucleotide microarrays," to identify a large number of genes highly overexpressed (made at high levels) in pancreatic cancer. Several of the new markers discovered by the team are now being brought to patient care as diagnostic markers, as prognostic markers, and as therapeutic targets. For example, the technology serial analysis of gene expression was developed here at Hopkins and was used to discover that the mesothelin protein is overexpressed in pancreatic cancer. Mesothelin has been reported to be useful as an aid to the interpretation of difficult cytology samples, as a blood marker, and as a therapeutic target in clinical trials.
The second approach the team has used is based on identifying mutations (DNA changes) that are only present in cancer cells. These cancer-specific mutations are extremely powerful tools, and have formed the basis of a blood test developed by the team at Hopkins for the earlier detection of cancer. Our goal is that one day asymptomatic individuals will go to their doctor for an annual check-up and this check-up will include a blood test that will detect any cancers early, while the cancers are curable.
Immune Therapies ▼
Immunotherpy is emerging as wonderfully effective for lung and certain other cancers. While immunotherapy has not proven to be effective against pancreatic cancer, Dr. Elizabeth Jaffee and colleagues are working on new immune modulating therapies and vaccines that, hopefully, will one day form the basis of new therapies.
Classification of Pancreatic Neoplasms ▼
By integrating molecular analyses with how cancers look under the microscope (tumor morphology) the team at Hopkins has also identified new types of cancer of the pancreas that have specific treatments. For example, the team discovered medullary cancer of the pancreas.
Recent Recognition/Awards ▼
Members of the Johns Hopkins Pancreatic Cancer have received numerous awards, including awards for being the most highly cited Pancreatic Cancer scientists in the world. Being highly cited means that our colleagues refer to our work when they publish scientific papers. But the team is most proud of the three Team Science Awards team members have received from the American Association for Cancer Research (AACR). The AACR Team Science Award recognizes a team of scientists for their "innovative and meritorious scientific work that has advanced or will likely advance cancer research, detection, diagnosis, prevention or treatment." In 2013 the team received this award for advances made in the fight against pancreatic cancer, in 2017 for advances made in developing an early detection ("liquid biopsy") test, and in 2020 for contributions to the national effort to define the molecular alterations that characterize cancer (the "TCGA").
Presentations by Our Medical Illustrators ▼
The research and clinical team collaborate closely with the Department of Art as Applied to Medicine here at Johns Hopkins. Our art students have created a number of research presentations and medical illustrations as part of our efforts to educate the public.
Our Pancreas Research Discoveries

2020
Dr. Kathy Burns and her team published an exciting finding in the journal Nature Structural and Molecular Biology. They study so called "repetitive elements" in the genome and found that a particular repetitive element, Line-1, when activated, can make cells very sensitive to certain treatments. Remarkably, Line-1 activation is very common in pancreatic cancer. Dr. Burns' work therefore suggests a completely novel approach to targeting pancreatic cancer. Although years away from being applied to patients, it is gratifying to see such promising fundamental progress.
Dr. Goggins and colleagues examined the SEER (Surveillance, Epidemiology and End Results) database for clinical trends in patients with pancreatic cancer in the United States. Remarkably, they found that more and more patients are being diagnosed early, with low stage (less advanced) disease. They found that low stage patients were more likely than high-stage (advanced disease) patients to carry insurance and to be white. While the finding that more low stage cancers are being detected is exciting, the study also highlights national inequities in the care of Blacks and those without insurance.

2019
Scientists in the Sol Goldman Center published over 25 papers in 2019. Here we highlight just two of them.
Elliot Fishman and colleagues applied "artificial intelligence," also known as "deep learning," and "radiomics" to CT scans of the pancreas (https://pubmed.ncbi.nlm.nih.gov/31492412/ and https://pubmed.ncbi.nlm.nih.gov/31012758/). The goal was of his team's work is to create an algorithm that checks CT scans looking for small pancreatic cancers that a human radiologist would miss. This would allow for the earlier detection of many small curable cancers. Using the method of "radiomics," Fishman and his team were able to identify sixty of sixty pancreatic cancers tested. The project, called the "FELIX Project," is generously supported by the Lustgarten Foundation.
A second research success that we would like to highlight relates to cystic tumors of the pancreas. Some cysts (fluid filled sacs) in the pancreas are precancerous lesions, and represent an opportunity to treat curable precancers before they become incurable invasive cancers. An example of this would be an Intraductal papillary mucinous neoplasm (IPMN) with high-grade dysplasia. Other cysts, such as "serous cysts," are harmless. The risk is that these harmless cysts would be mistaken for a potentially harmful one, and patients over treated. Dr. Lennon and colleagues reported in the journal Science Translational Medicine, a new test that can be applied to fluid removed from a cyst in the pancreas that can help clinicians distinguish harmless cysts from potentially harmful cysts. Dr. Eshleman and his team at Hopkins are now working to make this new test available to patients seen at Hopkins.

2018
2018 was a great year for scientists in the Sol Goldman Center. The team made a number of significant discoveries, a few of which are highlighted below.
Dr. Michaël Noë and colleagues reported how pancreatic cancer grows in three dimensions. Combining the novel techniques called "clearing" with "light sheet microscopy," the team reported that pancreatic cancers don’t grow randomly as they invade into tissues. Instead, the cancers seem to seek out blood vessels (veins), grow along side of them, and then invade into the veins. This finding is critically important because it may explain why pancreatic cancer is so aggressive. Pancreatic cancer cells that enter veins can then easily spread to the liver. Indeed, spread to the liver (liver metastases) are a major problem for patients with pancreatic cancer.
Also in 2018, Michael Goggins and colleagues, reported the discovery that inherited mutations in the CPA1 and CPB1 genes increase the risk of pancreatic cancer. These genes usually are associated with the development of pancreatitis. The findings by Goggins and colleagues, therefore adds to the growing body of evidence linking pancreatitis to the development of pancreatic cancer.
2017
Scientists in the Sol Goldman Center reported a number of significant advances in 2017. R. Hruban helped lead the effort by National Institutes of Health (NIH) to identify all of the genetic changes (DNA mutations) that drive pancreatic cancer. This team science effort, called the "TCGA," was reported in the journal Cancer Cell. Over 150 pancreatic cancers were studied at the DNA and RNA levels, defining the molecular landscape of pancreatic cancer. This study is important as it not only identifies the drivers of pancreatic cancer, but it also identifies genetic changes that can be used to detect pancreatic cancers, and, in some instances, the genetic changes may be targets for personalized therapies.
A nice demonstration of the potential power of the TCGA's effort, is a second study from the Goldman Center. In a paper published in the Proceedings of the National Academy of Sciences, Dr. Anne Marie Lennon and colleagues looked for mutations (genetic changes) in the KRAS gene in blood samples taken from 221 patients with resectable pancreatic cancer and 182 control patients without known cancer. KRAS was chosen because it is the gene most frequently targeted in pancreatic cancer. KRAS mutations were detected in the blood of 66 of the patients with pancreatic cancer, and every mutation found in the blood was identical to the mutation found in the patient’s primary pancreatic cancer (100% concordance). Dr. Anne Marie Lennon and colleagues then added protein biomarkers to here blood test and were able to detect two-thirds of the pancreatic cancers. Only one of the 182 blood samples from the controls without cancer was positive for any of the DNA or protein biomarkers. This combinatorial approach may prove useful for the earlier detection of pancreatic cancer.
Research Discoveries Archives
Highlighted below are selected research advances from the team at Johns Hopkins.
2016 ▼
Sequencing Familial Pancreatic Cancer Genomes
In a paper published in Cancer Discovery (February 2016), Nick Roberts, DVM, PhD, from the Sol Goldman Pancreatic Cancer Research Center reported the results of the largest ever sequencing study of familial pancreatic cancer. In a wonderfully collaborative multi-institutional study, Dr. Roberts and colleagues sequences the genomes of over 650 people with familial pancreatic cancer. They found that familial pancreatic cancer is remarkably heterogeneous. While previously known familial pancreatic cancer genes were identified (such as BRCA1, BRCA2, PALB2, ATM and p16/CDKN2A), most of the other candidate familial pancreatic cancer genes only explained a few families. There doesn’t appear to be one gene that explains all of familial pancreatic cancer, instead, many genes each explain only a few percent of familial pancreatic cancers. What does this mean for families? It means that in the future genetic counselors will not be testing high-risk patients for just one "familial pancreatic cancer gene." Instead, future tests will have to incorporate testing for panels of genes.
Reference:
Roberts NJ, Norris AL, Petersen GM, Bondy ML, Brand R, Gallinger S, Kurtz RC, Olson SH, Rustgi AK, Schwartz AG, Stoffel EM, Syngal S, Zogopoulos G, Ali SZ, Axilbund J, Chaffee KG, Chen YC, Cote ML, Childs EJ, Douville C, Goes FS, Herman JM, Iacobuzio-Donahue C, Kramer M, Makohon-Moore A, McCombie RW, McMahon KW, Niknafs N, Parla J, Pirooznia M, Potash JB, Rhim AD, Smith AL, Wang Y, Wolfgang CL, Wood LD, Zandi PP, Goggins M, Karchin R, Eshleman JR, Papadopoulos N, Kinzler KW, Vogelstein B, Hruban RH, Klein AP. Cancer Discov. February 2016.
Note: This study was generously funded with the support of Susan Wojcicki and Dennis Troper. Several of the participants in this study, including Dr. Hruban, receive royalty payments from Myriad Genetics for the PalB2 invention.
2015 ▼
Classification of Precancers
An international team of pathologists met at the Sol Goldman Pancreatic Cancer Research Center to examine the classification system for precancerous lesions in the pancreas. The group included participants from Japan, Europe and North America. After reviewing the "state of the art," the group proposed a simplified classification scheme that changes the previous three-tier grading system for precursors to a two-tier system. It is hoped that this simplified system will be easier for clinicians to apply in their day to day practice, and it will therefore improve patient care.
Reference:
Basturk O, Hong SM, Wood LD, Adsay NV, albores-Saavedra J, Biankin AV, Brosens LA, Fukushima N, Goggins M, Hruban RH, Kato Y, Klimstra DS, Klöppel G, Krasinskas A, Longnecker DS, Matthaei H, Offerhaus GH, Shimizu M, Takaori K, Terris B, Yachida S, Esposito I, Furukawa T. A revised classification system and recommendations from the Baltimore consensus meeting for neoplastic precursor lesions in the pancreas. Am J Surg Pathol. 39:1730-41, 2015.
Pancreatic Cancer that has Spread to the Lungs
T. Wangiam and colleagues reported in the journal Oncotarget that some patients with pancreatic cancer who develop metastases that are limited to the lung may be able to achieve longer survival. In the past doctors assumed that any spread (metastasis) of pancreatic cancer portended the patient’s death. Here, Wangiam and colleagues show that not all metastases are the same. Some patients with lung metastases can do well.
Reference:
Wangjam T, Zhang Z, Zhou XC, Lyer L, Faisal F, Soares KC, Fishman E, Hruban RH, Herman JP, Laheru D, Weiss M, Li M, De Jesus-Acosta A, Wolfgang CL, Zheng L. Resected pancreatic ductal adenocarcinomas with recurrence limited in lung have a significantly better prognosis than those with other recurrence patterns. Oncotarget. 6:36903-10, 2015.
Jumping Genes in Pancreatic Cancer
In two remarkable studies, Drs. N. Rodic and S. Solyom from the Sol Goldman Pancreatic Cancer Research Center reported that transposons (also known as "jumping genes") may play a role in the development of pancreatic cancer. Transposons were discovered years ago by scientists studying maize corn. Here Drs. Rodic and Solyom show how this same cellular process can lead to cancer when it goes a rye. What does this mean to patients with pancreatic cancer? Right now this is purely a "basic science" discovery that adds to the growing body of information on what can cause pancreatic cancer to develop in one person and not another. It has hoped that, in turn, a better understanding of the causes of pancreatic cancer will lead to new was to diagnose and treat this disease.
References:
Rodic N, Steranka JP, Makohon-Moore A, Moyer A, Shen P, Sharma R, Kohutek ZA, Huang CR, Ahn D, Mita P, Taylor MS, Barker NJ, Hruban RH, Iacobuzio-Donahue CA, Boeke JD, Burns KH. Retrotransposon insertions in the clonal evolution of pancreatic ductal adenocarcinoma. Nat Med. 21:1060-4, 2015.
Ewing AD, Gacita A, Wood LD, Ma F, Xing D, Kim MS, Manda SS, Abril G, Pereira G, Makohon-Moore A, Looijenga LH, Gillis AJ, Hruban RH, Anders RA, Romans KE, Pandey A, Iacobuzio-Donahue CA, Vogelstein B, Kinzler KW, Kazazian HH, Solyom S. Widespread somatic L1 retrotranspostion occurs early during gastrointestinal cancer evolution. Genome Res. 25:1536-45, 2015.
DNA Analysis of Cyst Fluid Can be used to Classify Pancreatic Cysts
Dr. Anne Marie Lennon reported a major advance in the diagnosis of pancreatic cysts in the journal Gastroenterology. Some pancreatic cysts are potential precancerous lesions and they represent an opportunity for early detection and early treatment. Other types of pancreatic cysts are completely harmless, and they represent a potential risk of over treatment (if all of them were removed because doctors thought they were the precancerous type). In an international collaborative effort, Dr. Lennon and colleagues sequenced the DNA in fluid removed from cysts and showed that the DNA changes in the cyst fluid could be used to predict the type of cyst. For example, GNAS and KRAS gene mutations suggest that the cyst is a mucin-producing cyst (an IPMN or MCN) which can be a precursor cyst, while VHL gene mutations suggest that the cyst is a serous cystic neoplasm (a usually harmless type of cyst). Dr. Lennon and colleagues are now working to validate their findings in a larger series of cases. They hope to make this a clinically available test.
Reference:
Springer S, Wang Y, Mokin MD, Masica DL, Jiao Y, Kinde I, Blackford A, Raman SP, Wolfgang CL…Goggins Ms, Canto MI, Ahuja N, Hirose K, Makary M, Weiss MJ, Cameron J, Pittman M, Eshleman JR, Diaz LA, Papadopoulos N, Kinzler KW, Karchin R, Hruban RH, Vogelstein B, Lennon AM. A combination of molecular markers and clinical fetaures improve the classification of pancreatic cysts. Gastroenterology. 149:1501-10, 2015.
Long-term Survivors
Dr. Marco dal Molin reported in Clinical Cancer Research an in-depth study of the cancers from patients with pancreatic cancer who survived long-term (greater than five or ten years). Dr. dal Molin and colleagues sequenced all known human genes (the "exomes") in a series of pancreatic cancers and compared the results of this sequencing with the sequencing results of pancreatic cancers resected from patients who survived only short-term after their surgery. Remarkably, the scientists were not able to identify significant differences in cancers from the two groups of patients. What does this mean? It means that there isn’t a simple "one gene" explanation for why some patients survive long-term. The reasons are likely to be complex, and may include factors such as the strength of the immune system.
Reference:
dal Molin M, Zhang M, de Wilde RF, Ottenhof NA, Rezaee N, Wolfgang CL, Blackford AL, Vogelstein B, Kinzler KW, Papadopoulos N, Hruban RH, Maitra A, Wood LD. Very long-term survival following resection for pancreatic cancer is not explained by commonly mutated genes: results of whole-exome sequencing analysis. Clin Cancer Res. 21:1944-50, 2015.
2014 ▼
Advances Made in a Blood Test for Pancreatic Cancer
In the February 19, 2014 issue of Science Translational Medicine (Sci Transl Med. 2014 Feb 19;6(224):224ra24), Bettegowda and colleagues in the Sol Goldman Pancreatic Cancer Research center at Johns Hopkins report on an exciting approach to the detection of pancreatic cancer. Bettegowda and colleagues applied cutting edge DNA sequencing to blood samples from a large number of patients with a number of different cancers. They found that many cancers, even some small curable cancers, shed mutant DNA into the blood. This mutant DNA circulating in the blood is called "circulating tumor DNA," or ctDNA for short. The team at Hopkins was able to show that ctDNA is detectable in >80% of patients with advanced pancreatic cancer, and close to half of the patients they studied with early, surgically resectable pancreatic cancers. There is more work to be done, but this study, we believe, represents a significant advance towards the development of a blood test for pancreatic cancer.
Multidiciplinary Cyst Clinic
As the complexity of diseases grows, more and more patients are seeking treatment at specialized centers of excellence such as Johns Hopkins. At these centers patients are often offered "multidisciplinary" care. This means that rather than just being evaluated by a physician from one specialty, patients' cases are evaluated by a team of doctors from multiple specialties. The team at Johns Hopkins established one of the first multidisciplinary clinics for the management of patients with pancreatic cysts. In the Annals of Surgical Oncology, Dr. Lennon and colleagues from Hopkins report on the impact that this cyst clinic has had.on improving patient care. Remarkably, the recommended management was changed for ~30% of the patients who were seen in the clinic. What does this mean for patients with a pancreatic cyst? The results suggest that patients may want to be evaluated at a major pancreatic center that has a multidisciplinary clinic dedicated to treating patients with pancreatic cysts.
Reference:
Lennon AM, Manos LL, Hruban RH, Ali SZ, Fishman EK, Kamel IR, Raman SP, Zaheer A, Hutfless S, Salamone A, Kiswani V, Ahuja N, Makary MA, Weiss MJ, Hirose K, Goggins M, Wolfgang CL. Role of a multidisciplinary clinic in the management of patients with pancreatic cysts: a single-center cohort study. Ann Surg Oncol. 21:3668-74, 2014.
Genetic Changes in Precancers
In a wonderful collaboration between US and Italian scientists, Dr. E. Amato and colleagues reported the results of extensive sequencing of intraductal papillary mucinous neoplasms (IPMNs) of the pancreas. The collaborative team sequenced 48 IPMNs and in so doing, they were able to confirm the genes that are frequently targeted in IPMNs (such as KRAS and GNAS), and they provided additional evidence that non-invasive IPMNs can give rise to invasive pancreatic cancer by showing that matched IPMNs and invasive cancers from the same patients had the same mutations. What does this mean for patients with an IPMN? It adds to the growing body of evidence that non-invasive curable precancerous lesions of the pancreas (IPMNs) should be detectable using DNA sequencing techniques before they progress to invasive cancer.
Reference:
Amato E, dal Molin M, Mafficini A, Yu J, Malleo G, Rusev B, Fassan M, Antonello D, Sadakari Y, Castelli, Zamboni G, Maitra A, Salvia R, Hruban RH, Bassi C, Capelli P, Lawlor RT, Goggins M, Scarpa A. Targeted next-generation sequencing of cancer genes dissects the molecular profiles of intraductal papillary neoplasms of the pancreas. J Pathol. 2014. (Awarded the Jeremy Jass Prize for Research Excellence in Pathology).
Blood test for Pancreatic Cancer
Early detection offers one of the best hopes for curing cancer. Dr. C. Bettegowda and colleagues from the Sol Goldman Pancreatic Cancer Research Center reported in the journal Science Translational Medicine that pancreatic cancers release abnormal (mutant) DNA into the blood stream (so called "circulating tumor DNA") and that this abnormal DNA can be detected. This is a significance advance in early detection because it suggested that a blood test could have the sensitivity and specificity needed for an early detection test. Further studies are needed to validate this approach. In the meanwhile the investigators are hard at work improving on their approach to early detection.
Reference:
Bettegowda C, Sausen M, Leary RJ, Kinde I,…Hruban RH, Wu J, Allen PJ, Schmidt CM, Choti MA, Velculescu VE, Kinzler KW, Vogelstein B, Papadopoulos N, Diaz LA. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 6:224ra24, 2014.
Sequencing Acinar Cancers
Not all tumors of the pancreas are "ductal adenocarcinomas," the type of tumor we usually mean when we refer to "pancreatic cancer." There are a number of variant tumors that can arise in the pancreas. One of the more aggressive of these is the acinar carcinoma. Acinar carcinomas only account for 1% of all cancers of the pancreas, but they can be very aggressive and are important to recognize. Jiao and colleagues from Johns Hopkins sequenced all known genes (the exomes) of a series of acinar carcinomas of the pancreas. They found that some of the genes targeted (mutated) in acinar carcinomas have been previously associated with familial pancreatic cancer. These genes include ATM, BRCA2 and PALB2. They also found that more than one-third of acinar carcinomas have potentially targetable genetic alterations, including mutations in the genes BRCA2, PALB2, ATM, BAP1, BRAF and JAK1.
Reference:
Jiao Y, Yonescu R, Offerhaus GJ, Klimstra DS, Maitra A, Eshleman JR, Herman JG, Poh W, Pelosof L, Wolfgang CL, Vogelstein B, Kinzler KW, Hruban RH, Papadopoulos N, Wood LD. Whole exome sequencing of pancreatic neoplasms with acinar differentiation. J Pathol. 232:428-35, 2014.
Outcome After Surgery
Surgical resection remains the best hope for curing patients with pancreatic cancer. In the journal HPB, Dr. He and colleagues report their results with over 2,500 surgical resections (Whipple resections). Whipple resections are typically done for one of four tumor types that can arise near the head of the pancreas- pancreas cancer, duodenqal cancer, bile duct cancer, or "ampullary" cancer. He and colleagues report operative mortality rates of only 1% (it seems high, but in the 1970s the operative mortality rate at some centers was 25%). Pancreatic cancer was associated with the worst survival (average 19 months) compared with cancers that arose in the ampulla (survival: 47 months), bile duct (survival: 23 months) and duodenum (survival: 54 months). What does it mean for a patient with a mass in the area of the pancreas? This paper highlights that surgery can be safe at specialized centers such as Johns Hopkins, and it shows that it is important to have resected tumors correctly classified.
Reference:
He J, Ahuja N, Makary MA, Cameron JL, Eckhauser FE, Choti MA, Hruban RH, Pawlik TM, Wolfgang CL. 2564 resected periampullary adenocarcinomas at a single institution: trends over three decades. HPB. 16:83-90, 2014.
2013 ▼
Follow-up After Intraductal Papillary Mucinous Neoplasm
More and more patients are undergoing surgery for an intraductal papillary mucinous neoplasm (IPMN) of the pancreas. IPMNs are curable lesions, but if left untreated, some will progress to invasive cancer. They therefore represent an opportunity for early detection and early treatment. He and colleagues from Johns Hopkins followed 130 patients who had an IPMN resected to see if they were at risk for a second tumor. Remarkably, 17% of the patients developed progressive disease in their remnant pancreas, and five of them developed an invasive pancreatic cancer. What does this mean? This study, and others like it, suggest that patients who have an IPMN surgically resected should be followed clinically after their surgery.
Reference:
He J, Cameron JL, Ahuja N, Makary MA, Hirose K, Choti MA, Schulick RD, Hruban RH, Pawlik TM, Wolfgang CL. Is it necessary to follow patients after resection of a benign pancreatic intraductal papillary mucinous neoplasm? J Am Coll Surg. 216:657-65, 2013.
A Genetic Approach to Detecting Intraductal Papillary Mucinous Neoplasms
Intraductal papillary mucinous neoplasms (IPMNs) can be precursors to invasive pancreatic cancer. The challenge can be detecting these precursor lesions. Dr. Kanda and colleagues report, in the journal Gut, a novel approach to detecting IPMNs. Patientrs undergoing upper endoscopy were given an injection of a drug called secretin. Secretin causes the pancreas to secrete fluid ("pancreatic juice"). This fluid was collected endoscopically and submitted to sequencing. Dr. Kanda and colleagues found that a DNA signature (GNAS mutations) can be detected in pancreatic juice samples from patients with an IPMN. This study suggests a new approach to developing a test for IPMNs- sequencing secretin stimulated pancreatic juice samples.
Reference:
Kanda M, Knight S, Topazian MD, Syngal S, Farrell J, Lee JH, Kamel I, Lennon AM, Borges M, Young A, Jujiwara S, Seike J, Eshleman J, Hruban RH, Canto M, Goggins M. Mutant GNAS detected in duodenal collections of secretin-stimulated pancreatic juice indicates the presence or emergency of pancreatic cysts. Gut. 62:1024-33, 2013.
2012 ▼
Younger Patients with Pancreatic Cancer
Most pancreatic cancers arise in elderly patients. Dr. He and colleagues in the Sol Goldman Pancreatic Cancer Research Center recently asked the question- "how do younger patients do after surgery?" Dr. he and colleagues report the results on 75 patients with pancreatic cancer who were ≤45 years old and who underwent surgery to have their tumor removed. They found, perhaps not surprisingly, that younger patients had fewer complications and lived longer after surgery than did older patients.
Reference:
He J, Edil GH, Cameron JL, Schulick RD, Hruban RH, Herman JM, Zheng L, Iacobuzio-Donahue C, Ahuja N, Pawlik TM, Wolfgang CL. Young patients undergoing resection of pancreatic cancer fare better than their older counterparts. J Gastrointest Surg. 17:339-44, 2012
Familial Pancreatic Cancer
Pancreatic cancer runs in some families. Inherited gene mutations in specific genes (such as BRCA2 and p16/CDKN2A) explain some families. In other families the gene responsible for familial pancreatic cancer is not known. Dr. N. Roberts and colleagues studied a number of families in which multiple family members had been diagnosed with pancreatic cancer. In several of these families they found that inherited (germline) mutations in a gene called ATM could explain the aggregation of pancreatic cancer in the family. What does it mean for me? This finding suggests that individuals with a strong family history may benefit from genetic testing for an inherited mutation in the ATM gene.
Reference:
Roberts NJ, Jiao Y, Yu J, Kopelovich L, Petersen GM, Bondy ML, Gallinger S, Schwartz AG, Syngal S, Cote ML, Axilbund J, Schulick R, Ali SZ, Eshleman JR, Velculescu VE, Goggins M, Vogelstein B, Papadopoulos N, Hruban RH, Kinzler KW, Klein AP. ATM mutations in patients with hereditary pancreatic cancer. Cancer Discov. 2:41-6, 2012.
Screening for Pancreatic Cancer
Early detection offers one of the best hopes for curing tumors of the pancreas. In a multi-center collaborative effort, Dr. M. canto and colleagues screened 225 asymptomatic high-risk (carriers of a gene known to predispose to pancreatic cancer or a strong family history of pancreatic cancer)adults using computed tomography (CT), magnetic resonance imaging (MRI), and endoscopic ultrasonography (EUS). Remarkably 82 intraductal papillary mucinous neoplasms and three pancreatic neuroendocrine tumors were detected. This study helps establish that screening asymptomatic individuals is possible. It has yet, however, been shown that such screening will save lives. Further, much larger, studies are needed.
Reference:
Canto MI, Hruban RH, Fishman EK, Kamel IR, Schulick R, Zhang Z, Topazian M, Takahashi N, Fletcher J, Petersen G, Klein AP, Axilbund J, Griffin C, Syngal S, Saltzman JR, Mortele KJ, Lee J, Tamm E, Vikram R, Bhosale P, Margolis D, Farrell J, Goggins M. Frequent detection of pancreatic lesions in asymptomatic high-risk individuals. Gastroenterology. 142:796-804, 2012.
2011 ▼
Sequencing Pancreatic Cysts
Some lesions in the pancreas produce cysts. Cysts are fluid-filled collections- kind of like a water balloon. Four different types of tumors commonly produce cysts in the pancreas. These include intraductal papillary mucinous neoplasms (IPMNs), mucinous cystic neoplasms (MCNs), solid-pseudopapillary neoplasms (SPNs) and serous cystadenomas (SCNs). SCNs are virtually always benign, SPNs are malignant (they can spread to other organs), and IPMNs and MCNs are precancerous lesions. Some MCNs and IPMNs, if left untreated, will progress to pancreatic cnacer. Wu et al sequenced all known human genes (the exomes) of a large series of clinically well-characterized cystic tumors of the pancreas and found that each cyst type has a characteristic pattern of genetic changes (mutations). SCNs harbor VHL mutations, SPNs beta-catenin mutations, MCNs harbor KRAS, RNF43, TP53 and p16 mutations, and IPMNs harbor GNAS, KRAS, RNF43, TP53 and p16 mutations. Why is this important? These findings suggest that DNA-based genetic tests can be developed that can help tell the harmful cysts apart from the potentially harmful cysts.
References:
Wu J, Jiao Y, dal Molin M, Maitra A, de Wilde RF, Wood LD, Eshleman JR, Goggins MG, Wolfgang CL, Canto MI, Schulick RD, Edil BH, Choti MA, Adsay V, Klimstra DS, Offerhaus GJ, Klein AP, Kopelovich L, Carter H, Karchin R, Allen PJ, Schmidt CM, Naito Y, Diaz LA, Kinzler KW, Papadopoulos N, Hruban RH, Vogelstein B. Whole-exome sequencing of neoplastic cysts of the pancreas reveals recurrent mutations in components of ubiquitin-dependent pathways. Proc Natl Acad Sci. 108:21188-93, 2011.
Wu GJ, Matthaei H, Maitra A, Dal Molin M, Wood LD, Eshleman J, Goggins M, Schulick R D, Edil BH, Wolfgang CL, Klein AP, Diaz, Jr. LA, Allen PJ, Schmidt CM, Kinzler KW, Papadopoulos N, Hruban RH, Vogelstein B. Recurrent GNAS mutations define an unexpected pathway for pancreatic cyst development. Sci Transl Med. 3:92ra66, 2011.
Sequencing Pancreatic Neuroendocrine Tumors
Pancreatic neuroendocrine tumors (PanNETs) account for 15% of malignant tumors of the pancreas. PanNETs, although less aggressive than the more common adenocarcinomas of the pancreas, are fully malignant tumors. In order to understand the fundamental genetics driving the development of PanNETs, Jiao and colleagues at Johns Hopkins sequenced the exomes (all of the known coding genes) of a series of clinically well-characterized PanNETs. The results were dramatic. In addition to confirming previous observations that the MEN1 gene is frequently targeted in PanNETs, the investigators discovered a new cancer pathway in which mutations in the genes DAXX or ATRX cause the "alternative lengthening of telomeres" in the tumors. They also found therapeutically potentially targetable mutations in "mTOR pathway" genes in ~15% of PanNETs. This study is important because it opens up this new cancer pathway to study and because it identifies a new approach to "personalized medicine" for patients with a PanNET.
References:
Jiao Y, Shi C, Edil BH, de Wilde RF, Klimstra DS, Maitra A, Schulick RD, Tang LH, Wolfgang CL, Choti MA, Velculescu VE, Diaz LA, Vogelstein B, Kinzler KW, Hruban RH, Papadopoulos N. DAXX/ATRX, MEN1 and mTOR pathway genes are frequently altered in pancreatic neuroendocrine tumors. Science. 331:1199-203, 2011.
Heaphy CM, de Wilde RF, Jiao Y, Klein AP, Edil BH, Shi C, Bettegowda C, Rodriguez FJ, Eberhart CG, Hebbar S, Offerhaus JA, McLendon R, Rasheed BA, He Y, Yan H, Bigner DD, Oba-Shinjo SM, Nagahashi Marie SK, Riggins GJ, Kinzler KW, Vogelstein B, Hruban RH, Maitra A, Papadopoulos N, Meeker AK. Altered telomeres in tumors with ATRX and DAXX mutations. Science. 333:425, 2011.
Personalized Therapy
One of the goals of sequencing cancers is to identify patient-specific mutations that could be exploited to develop individualized therapies. Villarroel and colleagues have done just that. They identified a genetic change (PALB2 mutation) in a pancreatic cancer that caused the patients cancer to be exquisitely sensitive to a specific drug (mitomycin C). Although just one case, it does serve as a wonderful example of the potential power of individualized therapy.
Reference:
Villarroel MC, Rajesh Kumar NV, Garrido-Laguna I, De Jesus-Acosta A, Jones S, Maitra A, Hruban RH, Eshleman JR, Klein AP, Laheru D, Donehower RC, Hidalgo M. Personalizing cancer treatment in the age of global genomic analyses: PALB2 gene mutations and the response to DNA damaging agents in pancreatic cancer. Mol Cancer Ther. 10:3-8, 2011.
Statement of conflict of interest:
Dr. Hruban and several other authors on this study receive royalty payments from Myriad Genetics for the PALB2 invention.
2010 ▼
Defining a Window of Opportunity for Early Detection
It is hard to imagine going back in time to determine the life history of a cancer, but Dr. Yachida and colleagues have done just that. By sequencing multiple different tumors from the same patient, they were able to estimate when and where each of the genetic changes they identified occurred. Surprisingly, they found that it can take many years for an invasive pancreatic cancer to develop. This study is important because it suggests that there is a large window of opportunity for the early detection of pancreatic cancer.
Reference:
Yachida S, Jones S, Bozic I, Antal t, Leary R, Fu B, Kamiyama M, Hruban RH, Eshleman JR, Nowak MA, Velculescu VE, Kinzler KW, Vogelstein B, Iacobuzio-Donahue CA. Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature. 467:1114-7, 2010.
2009 ▼
Precancers in Patients with a Family History
One of the first steps in developing an early detection test for a cancer is understanding the precancerous lesions from which the cancers arise. Dr. C. Shi and colleagues carefully studied the pancreases resected from a series of patients with a strong family history of pancreatic cancer and found that individuals with a strong family history have many more precancerous lesions in their pancreas than do patients without a family history. This study suggests that it may be easier to identify precancerous lesions early in individuals with a strong family history of the disease.
Reference:
Shi C, Klein AP, Goggins M, Maitra A, Canto M, Ali S, Schulick R, Palmisano E, Hruban RH. Increased prevalence of precursor lesions in familial pancreatic cancer patients. Clin Cancer Res. 15:7737-43, 2009.
Cancer Risk in Families
Approximately 10% of individuals with pancreatic cancer have a family history of the disease. Indeed, news reports suggest that former President Jimmy Carter has a strong family history of pancreatic cancer. Wang and colleagues followed a large series of individuals with a strong family history of pancreatic cancer and found that they are significantly more likely than the general public to develop cancer, including pancreatic cancer, themselves. This study identifies a population (individuals with a family history of pancreatic cancer) who might benefit from early detection screening efforts.
Reference:
Wang L, Brune KA, Visvanathan K, Laheru D, Herman J, Wolfgang C, Schulick R, Cameron JL, Goggins M, Hruban RH, Klein AP. Elevated cancer mortality in the relatives of pancreatic cancer patients. Cancer Epidemiol Biomarkers Prev. 18:2829-34, 2009.
Protein Markers
Some cancers produce abnormal amounts of specific proteins. These proteins are often then elevated in the blood of patients with that cancer, suggesting that proteins may be effective biomarkers for cancer. Dr. Harsha and colleagues carefully analyzed the literature on pancreatic cancer and they were able to compile a list of proteins that have been reported to be elevated in pancreatic cancer. They published this list as a resource for other investigators working on pancreatic cancer.
Reference:
Harsha HC, Kandasamy K, Ranganathan P, Rani S, Ramabadran S, Gollapudi S, Balakrishnan L, Dwivedi SB, Telikicherla D, Selvan LD, Goel R, Mathivanan S, Marimuthu A, Kashyap M, Vizza RF, Mayer FJ, DeCaprio JA, Srivastava S, Hanash SM, Hruban RH, Pandey A. A compendium of potential biomarkers of pancreatic cancer. PLOS Medicine Apr 7;6(4):e1000046, 2009.
Predicting Spread
Some pancreatic cancers are locally aggressive, invading local blood vessels, while other pancreatic cancers spread to other organs (they metastastasize). Dr. Iacobuzio-Donahue and colleagues report that mutations in a gene called “SMAD4” may explain this difference. Pancreatic cancers with intact SMAD4 appear to more likely be local problems, while pancreatic cancers with inactivated SMAD4 are more likely to spread to other oragns. Why is this important? It suggests that one day clinicians will be able to test pancreatic cancers for SMAD4 alterations and use the results in their clinical decision making.
Reference:
Iacobuzio-Donahue CA, Fu B, Yachida S, Luo M, Abe H, Henderson CM, Vilardell F, Wang Z, Keller JW, Banerjee P, Herman JM, Cameron JL, Yeo CJ, Halushka MK, Eshleman JR, Raben M, Klein AP, Hruban RH, Hidalgo M, Laheru D. DPC4 gene status of the primary carcinoma correlates with patterns of failure in patients with pancreatic cancer. J Clin Oncol. 27:1806-13, 2009.
PALB2 and Familial Pancreatic Cancer
Approximately 10% of individuals with pancreatic cancer have a family history of the disease. Jones and colleagues discovered one of the genes which, when inherited, can cause pancreatic cancer to run in families. Using genetic sequencing, Jones and colleagues showed that inherited mutations (DNA changes) in the PALB2 gene increase the risk of pancreatic cancer. This suggests that some individuals, especially those with a family history of breast and/or pancreatic cancer may one day benefit from genetic testing.
Reference:
Jones S, Hruban RH, Kamiyama M, Borges M, Zhang X, Parsons DW, Lin JC, Palmisano E, Brune K, Jaffee EM, Iacobuzio-Donahue CA, Maitra A, Parmigiani G, Kern SE, Velculescu VE, Kinzler KW, Vogelstein B, Eshleman JR, Goggins M, Klein AP. Exomic sequencing identifies PALB2 as a pancreatic cancer susceptibility gene. Science. 324:217, 2009.
Statement of conflict of interest:
Dr. Hruban and several other authors on this study receive royalty payments from Myriad Genetics for the PALB2 invention.
2008 ▼
Methylation of Precancers
Intraductal papillary mucinous neoplasms (IPMNs) can be a precursor to invasive pancreatic cancer. This is similar to colon polyps and colon cancer. Dr. Hong and colleagues from the Sol Goldman Pancreatic Cancer Research Center studied the methylation (addition of an extra carbon to certain parts of the DNA) patterns in a series of IPMNs. They found that some genes are abnormally methylated in IPMNs. This study not only adds to our understanding of the biology of IPMNs, but it also suggests that abnormal methylation markers may one day be useful in detecting IPMNs.
Reference:
Hong SM, Kelly D, Griffith M, Omura N, Li A, Li CP, Hruban RH, Goggins M. Multiple genes are hypermethylated in intraductal papillary mucinous neoplasms of the pancreas. Mod Pathol. 21:1499-507, 2008.
Sequencing Pancreatic Cancers
S. Jones and colleagues, in a real tour de force, sequenced all known human genes (the exomes) of a series of well-characterized pancreatic cancers. For the first time, scientists were able to define all of the major mutations (DNA changes) in pancreatic cancer. This can be thought of as learning the enemies "battle plans," or looking at the "blueprint" of how cancer works.
Reference:
Jones S, Zhang X, Parsons DW, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Kamiyama H, Jimeno A, Hong SM, Fu B, Lin MT, Calhoun ES, Kamiyama M, Walter K, Nikolskaya T, Nikolsky Y, Hartigan J, Smith DR, Hidalgo M, Leach SD, Klein AP, Jaffee EM, Goggins M, Maitra A, Iacobuzio-Donahue C, Eshleman JR, Kern SE, Hruban RH, Karchin R, Papadopoulos N, Parmigiani G, Vogelstein B, Velculescu VE, Kinsler KW. Core signaling pathways in human pancreatic cancers revealed by Global Genomic Analyses. Science. 321:1801-6, 2008.
Pancreatic Cysts are Common
Precancerous lesions in the pancreas can form small cysts (fluid-filled collections) in the pancreas. Pancreatic cysts therefore represent an opportunity for early detection. Laffan and colleagues examined over 2,800 CT scans of patients without any known pancreatic problems. Remarkably, they found that 2.6% of asymptomatic individuals have a cyst in their pancreas. This suggests that screening for asymptomatic pancreatic cysts may one day be a viable approach to the early detection of precancerous lesions in the pancreas.
Reference:
Laffan TA, Horton KM, KleinAP, Fishman EK, Johnson PT, Hruban RH. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol 191: 802-7, 2008.
Multidisciplinary Clinic for Pancreatic Cancer
One of the first multidisciplinary (multi-D) clinics for the management of patients with pancreatic cancer was established here at Johns Hopkins in 2006. Dr. T. Pawlik and colleagues evaluated the care that patients received at the multi-D clinic and found that multidisciplinary clinics can have real impact. 25% (1 in 4) patients had a change in their recommended management based on clinical review of their case by the multidisciplinary tumor board. This study suggests that complex diseases such as pancreatic cancer are often best managed at specialized high-volume centers and by multi-disciplinary teams of experts.
Reference:
Pawlik T, Laheru D, Hruban RH, Coleman J, Wolfgang DL, Campbell K, Ali S, Fishman EK, Schulick RD, Herman JM, and the Johns Hopkins Multidisciplinary Pancreas Clinic Team. Evaluating the impact of a single-day multidisciplinary clinic on the management of pancreatic cancer. Ann Surg Oncol. 15:2081-8, 2008.
2007 ▼
Predicting Risk in Families
Often people come to us with the question- "I have a strong family history of pancreatic cancer. What is my risk of getting the disease." Allison Klein and colleagues have developed a computer algorithm to answer this important question. The program can be used to estimate a person’s risk after their family tree (pedigree) has been entered. The program is available to trained genetic counselors.
Reference:
Wang W, Chen S, Brune KA, Hruban RH, Parmigiani G, Klein AP. PancPRO: risk assessment for individuals with a family history of pancreatic cancer. J Clin Oncol. 25:1417-22, 2007.
Inherited Breast Cancer Gene (BRCA2) Mutations
In addition to increasing the risk of breast and ovarian cancer, inherited (germline) mutations in the second breast cancer gene (BRCA2) increase the risk of pancreatic cancer. Dr. F. Couch and colleagues, in a collaborative multi-institutional study,examined a large number of individuals with a strong family history of pancreatic cancer, and found that inherited BRCA2 mutations account for 6% of moderate and high-risk pancreatic cancer families. Why is this important? This study is important because clinical testing for inherited BRCA2 gene mutations is now available. After appropriate genetic counseling, inviduals can be tested for a BRCA2 hene mutation and lives can be saved by breast and ovarian cancer screening.
Reference:
Couch FJ, Johnson MR, Rebe K, Brune K, deAndrade M, Goggins M, Gallinger S, Klein A, Petersen G, Hruban RH. The prevalence of BRCA2 mutations in familial pancreatic cancer. Cancer Epidemiol Biomarkers Prev. 16:342-6, 2007.
Precursor Lesions in the Pancreas
Dr. Kieran Brune and colleagues in the Sol Goldman Pancreatic Cancer Research Center carefully examined pancreases surgically resected from patients with a strong family history of the disease. The results were dramatic- many of these pancreases had multiple precancerous lesions and these precancerous lesions were microscopically associated with a very specific type of scaring called "lobulocentric atrophy." These findings are important because multifocal scarring (lobulocentric atrophy) is potentially clinically detectable using currently available imaging technologies (EUS). This suggests that screening for lobulocentric atrophy may one day become part of a screening test for early pancreatic cancer.
Reference:
Brune K, Abe T, Canto M, O’Malley L, Klein AP, Maitra A, Adsay NV, Fishman EK, Cameron JL, Yeo CJ, Kern SE, Goggins M, Hruban RH. Multifocal neoplastic precursor lesions associated with lobular atrophy of the pancreas in patients having a strong family history of pancreatic cancer. Am J Surg Pathol. 30:1067-76, 2006.
2006 ▼
Screening for Early Pancreatic Neoplasia in High-Risk Individuals
Dr. Marcia Canto and colleagues from Johns Hopkins report the results of the "CAPS 2" screening for early pancreatic cancer program in the June issue of Clinical Gastroenterology and Hepatology. Dr. Canto screened 72 individuals with a strong family history of pancreatic cancer, 6 patients with the Peutz-Jeghers Syndrome, and 149 controls using a combination of endoscopic ultrasound (EUS) and computerized tomography (CT scanning). If something abnormal was identified the patients also underwent endoscopic retrograde cholangiopancreatography (ERCP). All of the patients were asymptomatic. Remarkably, 8 of the patients were found to have a tumor in their pancreas (10% yield of screening); 6 patients had 8 benign intraductal papillary mucinous neoplasms (IPMNs), 1 had an IPMN that progressed to invasive ductal adenocarcinoma, and 1 had pancreatic intraepithelial neoplasia. Endoscopic ultrasound (EUS) and computerized tomography (CT scanning) also diagnosed 3 patients with 5 extrapancreatic neoplasms. Endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography abnormalities suggestive of chronic pancreatitis were more common in high-risk patients than in control subjects. From these studies, Dr. Canto concluded that screening EUS and CT diagnosed significant asymptomatic pancreatic and extrapancreatic neoplasms in high-risk individuals (people with a strong family history of pancreatic cancer and people with the Peutz-Jeghers Syndrome). Dr. Canto also concluded that abnormalities suggestive of chronic pancreatitis are identified more commonly in high-risk individuals. Dr. Canto plans to start "CAPS 3." More information about this research screening protocol will be posted on this web site as it becomes available.
Clin Gastroenterol Hepatol. May 5, 2006
DNA methylation alterations in the pancreatic juice of patients with suspected pancreatic disease
The biggest challenge of pancreatic cancer is to try to detect the cancer at an early stage when it can be surgically removed. Dr. Michael Goggins' Early Detection Laboratory is dedicated to identifying new markers for the early detection of pancreatic cancer. Just as there is mammography for breast cancer and the PSA test for prostate cancer, so too do we need a test for early pancreatic cancer. Scientists working in The Early Detection Laboratory at Johns Hopkins examined the DNA in pancreatic juice samples that were collected from pancreatic cancer patients to determine if the DNA from these samples showed an abnormal amount of methylation. Methylation is the addition of an additional carbon to specific areas of the DNA. Hypermethylation (or too much methylation) of certain genes will stop the genes from working properly. In particular, hypermethylation of genes whose normal function is to protect a cell from developing into a cancer (tumor suppressor genes) or whose function is to repair damaged DNA (mismatch repair genes) have been associated with the development of cancer. The scientists found that there was more methylation in the pancreatic juice samples collected from pancreatic cancer patients than there was in the samples collected from chronic pancreatitis patients and patients with no history of pancreatic disease. This finding is important because it suggests that the detection and quantification of methylated DNA in pancreatic juice may provide a promising approach to the diagnosis of pancreatic cancer.
Cancer Res. 66:1208-17, 2006
2005 ▼
Early Results Using Therapeutic Pancreatic Cancer Vaccine Show Promise
Researchers in the Sol Goldman Pancreatic Cancer Research Center in the Johns Hopkins Kimmel Cancer Center are encouraged by early results of a treatment vaccine for pancreatic cancer. At about two years into a study of 60 patients, the researchers report that 88 percent survived one year and 76 percent are alive after two years.
"Even though our results are preliminary, the survival rates are an improvement over most published results of pancreatic cancer treatment studies," says Daniel Laheru, assistant professor at the Johns Hopkins Kimmel Cancer Center. Laheru is expected to present his findings in a press briefing at a joint meeting of the American Association for Cancer Research/National Cancer Institute/European Organization for Research and Treatment of Cancer in Philadelphia on November 15.
Until recently, most studies have shown pancreatic cancer survival rates at about 63 percent one year after diagnosis and 42 percent at two years. The long-term outlook is more grim - only 15 to 20 percent of patients with local disease are alive at five years. "Since there is no universal standard for treating pancreatic cancer, it is difficult to make direct comparisons between all the studies," says Laheru.
In the current study, his team combined an immune-boosting vaccine with surgery and conventional postoperative chemotherapy and radiation. The vaccine, originally developed at Johns Hopkins, uses irradiated pancreatic cancer cells incapable of growing, but genetically altered to secrete a molecule called GM-CSF. The molecule acts as a lure to attract immune system cells to the site of the tumor vaccine where they encounter antigens on the surface of the irradiated cells. Then, these newly armed immune cells patrol the rest of the patient's body to destroy remaining circulating pancreatic cancer cells with the same antigen profile.
Patients get one vaccine injection eight to ten weeks after surgery, then four booster shots after chemotherapy and radiation. Laheru and his team completed enrolling patients in the study this past January. The average follow-up time is 32 months.
Jaffee and Laheru hope to begin multi-institutional studies in about a year. They are working with Hopkins pathologists from the Sol Goldman Pancreatic Cancer Research Center to analyze proteins from pancreatic cancer cells that may help them refine the vaccine's targets.
Proceedings, AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics, November 2005. (Abstract #2229, A Safety and Efficacy Trial of Lethally Irradiated Allogeneic Pancreatic Tumor Cells Transfected with the GM-CSF Gene in Combination with Adjuvant Chemoradiotherapy for the Treatment of Adenocarcinoma of the Pancreas).
Reaction of the Normal Pancreas to an Adjacent Pancreatic Cancer Provides Clues about Tissue Invasion and Detection.
Two papers from the Hopkins group help define the genes that are expressed (made) in the tissues adjacent to pancreatic cancer. In the first paper by Ricci and colleagues, the technique of in situ hybridization was used to determine the genes that are turned on in the body's response (called a stromal reaction) to an infiltrating cancer (analogous to the body trying to heal a wound). Importantly, Dr. Ricci found that the genes that are made in this stromal response to an invasive pancreatic cancer are related to how aggressively the tumor invades the surrounding pancreas, and not to the underlying biology of the tumor. Understanding how pancreatic cancers invade the normal pancreas and spread to other organs is a critical step to understanding how to interfere with this process. In the second paper by Fukushima and colleagues, gene expression profiling was used to better understand the gene expression patterns of pancreatic tissue adjacent to infiltrating pancreatic cancers as compared to pancreatic tissue adjacent to chronic pancreatitis. Dr. Fukushima found 20 different genes were overexpressed in pancreatic tissue adjacent to an invasive cancer compared to normal pancreatic tissue adjacent to chronic pancreatitis. These results demonstrate that some of the molecular alterations in normal pancreatic tissues that occur in response to adjacent infiltrating pancreatic ductal adenocarcinoma can provide a rich source of markers for detecting pancreatic cancer.
Cancer Biol Ther. 4:302-7, 2005
Mod Pathol. 18; 779-87, 2005
New Potential Target for Therapy
Dr. Anirban Maitra and colleagues at Johns Hopkins have identified a genetic change in pancreatic cancers that has potential therapeutic implications. MTAP is a gene on chromosome 9 and novel chemotherapeutic strategies exploiting the selective loss of MTAP function in cancers have been proposed. The MTAP gene is adjacent to the p16 gene and MTAP and p16 are frequently deleted from the DNA of pancreatic cancers. Dr. Maitra has found these deletions of the MTAP and p16 genes in 30% of pancreatic cancers, suggesting that selected patients with pancreatic cancer may benefit from therapies targeting this loss. Studies are now underway in animal models to test this potential new treatment approach.
Cancer Biol Ther. 15:83-6, 2005
Precursor Lesions of Pancreatic Cancer
Catching the Horse before It has Fled the barn
Three articles by Johns Hopkins scientists have expanded our knowledge of the precursor lesions which are thought to develop into invasive pancreatic cancers. Understanding the biology of these precursor lesions is of critical importance if we are to detect, and potentially treat, pancreatic cancer before it spreads. In the first article, Anirban Maitra and collegues comprehensively reviewed the various subtypes of precursor lesions that are known to progress to invasive pancreatic cancer. While Pancreatic Intraepithelial Neoplasia or "PanIN" is the prototype precursor lesion associated with the "usual" cancers (ductal adenocarcinomas), other larger precursor subtypes such as intraductal papillary mucinous neoplasms (IPMNs) and mucinous cystic neoplasms (MCNs) are being increasingly recognized with better imaging and screening techniques. The pancreatic cancers that arise in the context of these latter precursor lesions, particularly IPMNs, can have a different biology and outcome than the usual PanIN-associated invasive cancers. Therefore, it is important that pathologists who examine surgically removed pancreata are familiar with the histology of the various non-invasive precursors to invasive pancreatic cancers.
The second and third articles identify potential therapeutic targets in PanINs, the most common precursor lesion of pancreatic cancer. Inactivation of function of a critical gene that controls the cell cycle - p16 (CDKN2A) - is extremely frequent in invasive pancreatic cancers. In about a third of these cases, loss of p16 function occurs via deletion of both p16 gene copies (called "homozygous deletion" in genetic terminology) and is large enough to include a neighboring gene known as MTAP in the deletions. Complete loss of MTAP function can be exploited for therapy using drugs that selectively affects MTAP-negative pancreatic cancer cells without damage to normal tissues. Now, Dr. Hustinx and collegues have shown that even subsets of non-invasive precursor lesions (PanINs) harbor deletions of both copies of the MTAP gene. This is the first demonstration of a homozygous deletion in a PanIN lesion, and the authors have described a simple assay that will enable determining MTAP gene status in limited tissue materials, such as biopsy specimens. Why is this important? Compounds that selectively target MTAP-negative pancreatic cancers are already in clinical trials; if successful, one can envision extrapolating these trials to treat the precursors to invasive cancer before a cancer develops. The challenge will be in identifying patients with non-invasive, MTAP-negative precursor lesions who might potentially benefit from this therapy. With advances in molecular imaging and biopsy techniques, scientists are hopeful that this strategy will be actualized in the future.
In the third article, Dr. Prasad and colleagues performed the first large scale gene expression profiling of PanIN lesions using "gene chips". Johns Hopkins scientists were one of the first to comprehensively determine the gene expression profile of invasive pancreatic cancer, and the group at Hopkins has now extended this knowledge to precursor lesions as well. In order to isolate these tiny ductal lesions from surrounding normal tissues, the scientists used a technique called "laser capture microdissection". They found 49 genes that were expressed differentially compared to normal ductal epithelium. Of note, they found many of the overexpressed genes in PanINs are normally turned on by activation of the sonic hedgehog pathway during development, thereby confirming that abnormal activation of this pathway plays a role in both early and advanced pancreatic cancers. Hopkins scientists had previously demonstrated that the sonic hedgehog pathway is a powerful therapeutic target in invasive pancreatic cancers, and this current work provides rationale for investigating this line of therapy in the prevention of pancreatic cancers as well.
Why is this important to me? The studies of the MTAP gene are important because compounds that selectively target MTAP-negative pancreatic cancers are already in clinical trials; if successful, one can envision extrapolating these trials to treat the precursors to invasive cancer before a cancer develops. The challenge will be in identifying patients with non-invasive, MTAP-negative precursor lesions who might potentially benefit from this therapy. With advances in molecular imaging and biopsy techniques, scientists are hopeful that this strategy will be actualized in the future.
Adv Anat Pathol. 2005 Mar;12(2):81-91. PMID: 15731576
Mod Pathol. 2005 Jul;18(7):959-63. PMID: 15832197
Cancer Res. 2005 Mar 1;65(5):1619-26. PMID: 15753353
2004 ▼
New Technology Developed for the Early Detection of Pancreatic Cancer
There are no early warning signs of pancreatic cancer and there are no early detection tests. As a result, most patients are not diagnosed until after the cancer has spread. Just as there is a PSA test for prostate cancer, so too do we urgently need an early detection test for pancreatic cancer. Dr. James Eshleman at Hopkins has recently developed a new technology that can detect rare DNA mutations (alterations in the DNA sequence) even when these mutations are admixed with much larger numbers of normal DNA sequences (Nat Methods. 2004 Oct 21;1(2):141-147 ). The technology, called "LigAmp" detected the most common mutation found in pancreatic cancer (KRAS2 gene mutations) even when a single mutant KRAS2 gene was admixed with 1,000 normal genes. Dr. Eshleman and colleagues have further shown that LigAmp can be used to detect DNA mutations shed from pancreatic cancers in pancreatic juice samples.
Nat Methods. 1:141-7, 2004
Applying new bioinformatics technology to discover new markers of pancreatic cancer (November and December 2004)
The cloning of the human genome has opened the door to global analyses of gene expression in pancreatic cancer on a scale not imaginable a few years ago. These analyses can help identify literally hundreds of genes that are made at high levels by pancreatic cancer cells. All too often however, the analyses produce potentially interesting gene sequences but the identity of the gene for which these sequences code for has not been identified. Akhalesh Pandey at Johns Hopkins has used cutting edge bioinformatics tools to identify a number of exciting genes that are overexpressed in pancreatic cancer. These genes are potential targets for new therapies and for the early detection of pancreatic cancer.
Cancer Biology and Therapy November 2004
Cancer Biology and Therapy December 2004
New proteomic markers of pancreatic cancer found (September 2004)
Proteomics is the study of all of the proteins in a tissue or fluid. Dr. Akhelesh Pandey carried out a comprehensive characterization of the "pancreatic juice proteome" in patients with pancreatic adenocarcinoma. A total of 170 unique proteins were identified including known pancreatic cancer tumor markers (e.g., CEA, MUC1) and proteins overexpressed in pancreatic cancers (e.g., hepatocarcinoma-intestine-pancreas/pancreatitis-associated protein (HIP/PAP) and lipocalin 2). In addition, he identified a number of proteins that have not been previously described in pancreatic juice (e.g., tumor rejection antigen (pg96) and azurocidin). The proteins identified in this study will be further assessed for their potential as biomarkers for pancreatic cancer by quantitative proteomics methods or immunoassays.
J Proteome Res. Sep-Oct; 3(5):1042-55, 2004
Exploiting BRCA2 gene mutations to treat pancreatic cancer (August 2004)
Nine years ago, the Kern Laboratory found mutations of a new gene, called BRCA2. Soon, this laboratory and others working in other tumor systems found that mutations of the gene were often inherited, raising the risk for pancreatic, ovarian, and breast cancer when an individual inherits one bad copy of the gene. This was the second gene found to cause inherited breast cancer, thus leading to the gene name, BRCA2. Dr. Kern's postdoctoral fellow Michiel van der Heijden followed up on this earlier discovery and showed that that pancreatic cancer cells with BRCA2 gene mutations are especially susceptible to the anticancer drugs mitomycin and cis-platin. Based on this exciting finding, it may be possible in the future to recommend individualized therapeutic regimens for patients with these mutations. More research, and possibly even a clinical trial, in this new area are underway.
Am J Pathol. 165:651-7, 2004
Immune target for the treatment of pancreatic cancer discovered (August 2004)
Dr. Elizabeth Jaffee has developed a novel whole cell vaccine to treat patients with pancreatic cancer. She has previously found that this vaccine treatment produces an anti-tumor immune response in some patients. In the August issue of the Journal of Experimental Medicine, Dr. Jaffee reports that she has discovered a protein, mesothelin that appears to be responsible for the anti-tumor effect seen with the whole cell vaccine. Mesothelin is an antigen demonstrated previously by gene expression profiling to be up-regulated in most pancreatic cancers, and Dr. Jaffee found the consistent induction of CD8(+) T cell responses to mesothelin in patients who responded to the vaccine. This finding not only provides insight into the immune mechanisms underlying anti-tumor responses, but it is also hoped that it will lead to new "peptide" based vaccines that are cheaper and easier to administer than the whole cell vaccine.
Journal of Experimental Medicine, 2004
Using endoscopic ultrasound (EUS) to screen for early pancreatic cancer in asymptomatic patients (July 2004)
In the July issue of Clinical Gastroenterology Hepatology, Dr. Marcia Canto and colleagues from Johns Hopkins report the results of screening for pancreatic cancer in asymptomatic (patients without symptoms) individuals known to be at increased risk because of their family history. Endoscopic ultrasound (EUS) was used. In this technique a small tube with an ultrasound device at the end is inserted through the patient's nose and into the patient's stomach and duodenum. The ultrasound device can then be used to image the pancreas. Thirty-eight patients were screened in Dr. Canto's study and six pancreatic masses were found. Several of these patients went to surgery and one was found to have an early cancer and another a precancerous tumor (intraductal papillary mucinous neoplasm). Therefore, 5.3% or 1 in 20 patients was found to have a clinically important pancreatic mass. This study therefore represents the first step towards demonstrating that screening for early pancreatic cancer is possible.
Clin Gastroenterol Hepatol 2(7):606-21, 2004
The risk of pancreatic cancer increases if you have more relatives with pancreatic cancer (April, 2004)
Dr. Klein and colleagues followed 838 families who participate in the National Familial Pancreatic Tumor Registry at Johns Hopkins to determine how if new pancreatic cancers are more likely to develop in families in which more than one family member has been diagnosed with pancreatic cancer. Twenty-two new pancreatic cancer cases developed in these families after the family had entered the registry. Dr. Klein found that individuals with three or more first-degree relatives with pancreatic cancer (brothers, sisters, parents or children) had a 32-fold increased risk of developing pancreatic cancer. Individuals with two first-degree relatives with pancreatic cancer had a 6.5-fold increased risk. This increase in risk was even higher among family members who smoked cigarettes. The results of this study further establish that pancreatic cancer does cluster in families. Additionally, these results help to identify individuals who may benefit from screening for the early signs of pancreatic cancer once reliable screening tests are developed.
Cancer Research 64:2634-2638, 2004
Two potential new blood markers of pancreatic cancer (March and April 2004)
New blood markers for the early detection of pancreatic cancer are urgently needed. Just as there is a PSA test for prostate cancer, so too do we need a test for pancreatic cancer. Dr. Goggins' lab is dedicated to the discovery of these markers and in 2004 he reported the discovery of two new promising markers, osteopontin and MIC-1. These markers were identified in previous studies of gene expression using "gene chip" analysis of surgically resected cancers, and Dr. Goggins went on to show that both MIC-1 and osteopontin are released into the blood and that the blood levels of these markers are higher in patients with pancreatic cancer than they are in patients without cancer. Both markers were significantly better than the previous "gold standard" CA 19-9.
Cancer Epidemiol Biomarkers Prev. 13:487-91, 2004
Clin Cancer Res. 10(7):2386-92, 2004
Improved understanding of intraductal papillary mucinous neoplasms (IPMNs) of the pancreas (March 2004)
Intraductal papillary mucinous neoplasms (IPMNs) of the pancreas are being diagnosed with growing frequency, but these distinctive tumors of the pancreas have not been well-characterized. Dr. Goggins and coworkers used cutting edge oligonucleotide microarrays to analyze the genes made ("the gene expression profile") by a series of IPMNs. They identified four genes that appeared to be highly associated with the presence of an invasive adenocarcinoma. Notably, the expression of at least two of the four genes was observed in 73% of 22 invasive IPMNs but in none of 16 noninvasive IPMNs (P < 0.0001). These findings suggest that preoperative assessment of gene expression profiles may be able to differentiate invasive from noninvasive IPMNs. They have also performed a similar analyses on another type of tumor in the pancreas called "mucinous cystic neoplasm."
Am J Pathol. 164(3):903-14, 2004
Oncogene. Oct 18, 2004.
Series of advances made by Dr. Iacobuzio-Donahue's lab (Spring 2004)
Dr. Iacobuzio-Donahue recently published two exciting articles in Cancer Research. The first article, published in the December 15 issue (Cancer Research 2003; 63:8614-22) describes the largest, most comprehensive study to date of gene expression (the genes made) in pancreatic cancer. Close to 100 samples were analyzed using the most current gene chip (Affemetrix U133). Dr. Iacobuzio-Donahue and colleagues discovered 142 potential new markers of pancreatic cancer. Already, Dr. Koopmann has shown that one of these markers, called "osteopontin," is elevated in the blood of patients with pancreatic cancer (Cancer Epi Biomarkers Prev, 2004; 13:487-91) and Dr. Nichols has demonstrated that another of these markers, claudin 4, may be a useful therapeutic target (Am J Clin Pathol. 2004; 121:226-30).
In the second paper published by Dr. Iacobuzio-Donahue (Cancer Research 2004; 64:871-875) she describes the largest genetic analysis conducted to date of the DNA changes in pancreatic cancer. Dr. Iacobuzio-Donahue and colleagues conducted a large-scale "allelotypes" (an analysis of DNA losses in a cancer) on a series of pancreatic cancers and they discovered a number of hot spots of DNA alterations in pancreatic cancer. These hot spots will help other scientists identify the genes that are targeted for inactivation in pancreatic cancer. An understanding of these genes, in turn, may lead to a better understanding of why pancreatic cancer develops and how to treat it.
Cancer Res. 64: 871-875, 2004
Cancer Epidemiol Biomarkers Prev. 13:487-91, 2004
Clin Cancer Res. 10:1597-1604, 2004
Am J Clin Pathol. 121(2):226-30, 2004
2003 ▼
Mutations in the BRAF gene found in pancreatic cancer (October 2003)
It has become clear that pancreatic cancer is a disease caused by damage to the DNA (called mutations). The identification of which genes are mutated in pancreatic cancer provides insight into the fundamental nature of the disease. In the October issue of the American Journal of Pathology, Dr. Kern and colleagues report mutations in the BRAF and in the FBXW7 genes. It is hoped that a better understanding of the effects of these mutations will provide insight into why pancreatic cancer is so aggressive.
Am J Pathol. 163:1255-60, 2003
Determining the stage at which selected genes are made in tumors of the pancreas (September 2003)
Just as colon polyps give rise to invasive colon cancer, so too has it become clear that small non-invasive lesions in the pancreas (called PanINs) can give rise to invasive pancreatic cancer. These small non-invasive lesions in the pancreas are exciting, because they represent a curable stage of pancreatic cancer. Dr. Anirban Maitra at Johns Hopkins has studied a large series of "PanINs" and he has defined the stages at which different genes are made by the tumor cells. This finding is exciting because it identifies which genes are the best targets for the development of early detection tests, and which genes are the best targets for the treatment or prevention of early tumors of the pancreas.
Mod Pathol. 16:902-12, 2003
Improving the interpretation of small biopsies of the pancreas (September 2003)
It can be very difficult to biopsy the pancreas, and when the pancreas is biopsied often only a few cells are obtained. As a result, the diagnostic interpretation of pancreatic biopsies can be very difficult. Scientists at Johns Hopkins have identified a group of genes that are made at high levels by pancreatic cancer cells. They then showed that staining small biopsies for two of these markers, PSCA and mesothelin, can greatly improved the accuracy of diagnosis and therefore improve patient care.
Appl Immunohistochem Mol Morphol. 11:238-43, 2003
New cellular pathway found to be active in pancreatic cancer (September 2003)
Scientists at Johns Hopkins have discovered a cellular pathway that is activated in pancreatic cancer, a finding that provides a potential new way to treat pancreatic cancer. These findings are reported in the journal Nature (the September 14 advanced online publication can be accessed at www.nature.com/nature). This work was performed in the laboratory of Dr. Philip Beachy, who is a Member of the National Academy of Sciences, and a renowned developmental biologist at Johns Hopkins. Dr. Beachy and colleagues demonstrated that the "Hedgehog" pathway is abnormally turned on in many digestive tract tumors, including those of the pancreas. In addition, they have demonstrated that the administration of a drug known as cyclopamine that specifically blocks this pathway in cancer cells results in dramatic reduction of cancer growth. In a mouse model they showed complete and sustained reduction of the tumor following only two weeks of therapy with cyclopamine; most importantly, the mice did not appear to suffer any side effects from the therapy. Although application to humans is years away, the results of this study have potential implications for future treatment options in pancreatic cancers, and demonstrate how knowledge of underlying molecular abnormalities in tumors can lead to new therapies.
Nature
New Targets for Aberrant Methylation in Pancreas Cancer (July 2003)
Research by Norihiro Sato M.D., Ph.D. in the laboratory of Dr. Michael Goggins has led to the discovery of multiple genes that undergo silencing by DNA methylation (the addition of a carbon group to DNA) in pancreatic cancer. Knowledge of these genes provides us with a better understanding of the role of DNA methylation in pancreatic cancer development. The doctors also showed that these abnormally methylated genes can be detected in pancreatic juice from patients with pancreatic cancer and raising hopes that their detection could aid in the early diagnosis of pancreatic cancer.
Cancer Research (Volume 63, pages 3735-42)
Pancreatic Cancer Linked to Errant Reactivation of Embryo Cell Pathway (June 2003)
Research by Johns Hopkins Kimmel Cancer Center specialists has uncovered a novel pathway in the origin of pancreatic cancers. The "Notch" pathway, normally turned off in adults, can be turned on after injury to the pancreas.
The findings of Dr. Steven Leach et al. are reported in the June 23, 2003, issue of Cancer Cell.
Fanconi Gene Abnormalities in Pancreatic Cancer (May 2003)
Dr. Michiel van der Heijden and colleagues studied two of the Fanconi genes: FANCC and FANCG. Inherited and new mutations were found in a number of pancreatic cancers. Some of these mutations are inherited, meaning that these individuals had an increased risk of developing pancreatic cancer because they were born with these mutations in their DNA (they had inherited them from one of their parents. Dr. van der Heijden and colleagues had another interesting finding: three of the nine persons whose pancreas cancer had young onset (less than 50 years of age) had such mutations.
There are no easy tests for the kinds of Fanconi gene mutations now being studied by the researchers, but such tests may become available in the future. Such testing is likely to be of clinical importance. Cells that are defective in the Fanconi genes are known from other research to be highly sensitive to certain chemicals. If may be possible in the future to recommend a different therapeutic regimen for patients with these mutations. More research in this exciting new area is needed.
Cancer Research (Volume 63, 2585-2588)
Activin Abnormalities in Pancreatic Cancer (March 2003)
Activin receptors play an important "controlling" roll in normal pancreatic cells. Dr. Byungwoo Ryu and colleagues in the Kern Laboratory therefore studied the genes that respond to activin signals to uncover the ways in which the cells are regulated by activin. Using a high-density gene expression screen, they studied gene expression changes characteristic of activin. Some of the genes regulated include genes that directly control cell division. This work was published in the journal Cancer Biology & Therapy, (Volume 2, pages 164-70), and represents the largest study of gene responses to activin published to date.
Also working in Dr. Kern's lab, Dr. Paula Hempen and colleagues found mutations of another form of the activin receptor in pancreatic cancer cells, extending the numbers of tumors known to have abnormalities in the activin system. The newly discovered mutations are in the ACVR2 gene, the activin type 2 receptor. The ACVR2 gene mutations were found in nearly all gastrointestinal tumors that had defects in a DNA-repair pathway involved in familial forms of cancer, including families at high risk of colorectal, pancreatic, and endometrial cancers.
Cancer Research (Volume 63, pages 994-9)
Anti-Cancer Drug Can Lead to Cancer Invasion (February 2003):
Dr. Sato and colleagues reported an unexpected adverse effect of an anti-cancer drug that is used to remove "methyl" groups (carbon-hydrogen) from DNA. The authors found that this drug can inadvertently switch on certain genes (matrix metalloproteinases) and that the switching on of these genes can promote cancer invasion. This study shows that each therapy needs to be carefully evaluated, because therapies can have unanticipated side effects.
Journal of the National Cancer Institute (Volume 95, pages 327-30)
2002 ▼
Target of chemopreventive agents (August 2002)
One of the more exciting approaches to saving lives is preventing pancreatic cancer through the use of "chemopreventive" agents. Chemopreventive agents are drugs that are taken regularly and reduce one's risk of cancer. Cox-2 (also known as cyclooxygenase 2) is an enzyme made by cells that is a target for some chemopreventive drugs. In the August issue of the American Journal of Clinical Pathology, Dr. Maitra and colleagues from Johns Hopkins report that cyclooxygenase 2 is expressed (made by) small lesions in the pancreas called "pancreatic intraepithelial neoplasia." This is important because pancreatic intraepithelial neoplasia is believed to be the precursor to pancreatic cancer. The expression of cyclooxygenase 2 in pancreatic intraepithelial neoplasia lesions suggests that cyclooxygenase 2 inhibitors could be used to prevent the development of pancreatic cancer. Further work is needed, but clearly chemopreventive agents, such as cyclooxygenase 2 inhibitors, offer an exciting new approach to fight pancreatic cancer before it develops.
American Journal of Clinical Pathology(Volume 118, pages 194-201)
BRCA2 gene is important in familial pancreatic cancer (July 2002)
Investigators from Johns Hopkins found that 1 in 6 (17%) patients with a very strong family history of pancreatic cancer have inherited ("germline") mutations (changes) in the BRCA2 gene. The BRCA2 is also known as the second breast cancer gene. Although it has been known for years that BRCA2 was important in familial breast cancer, the importance of BRCA2 in familial pancreatic cancer is only now coming to light. Inherited mutations in BRCA2 are particularly common in the Ashkenazi Jewish population. The identification of a gene responsible for the familial aggregation of pancreatic cancer is important because at-risk family members can now be tested to see if they carry this gene.
Cancer Research (Volume 62, pages 3789-93)
Genetic alterations in solid-pseudopapillary tumors of the pancreas (April 2002):
Solid-pseudopapillary tumors are rare tumors of the pancreas that arise primarily in young women. They have a distinct appearance under the microscope and a much better prognosis than the more common ductal adenocarcinomas of the pancreas. Scientists at Johns Hopkins studied the fundamental genetic (DNA) changes in a series of solid-pseudopapillary tumors of the pancreas and found that they almost all have mutations (DNA changes) in a particular gene called Beta-catenin. By contrast, usual ductal adenocarcinomas of the pancreas almost never have Beta-catenin mutations.
It can sometimes be difficult in a small biopsy or even in a resected specimen to distinguish between the various types of tumors that arise in the pancreas. This discovery suggests that the presence or absence of Beta-catenin mutations in a tumor can be used to distinguish between solid-pseudopapillary tumors (which have a very good prognosis) and usual ductal adenocarcinomas (which do not have a good prognosis).
American Journal of Pathology (Volume 160, pages 1361-1369)
Genetic alterations in acinar cell carcinomas of the pancreas (March 2002)
Acinar cell carcinomas are rare malignant tumors of the pancreas. They are microscopically different from the more common "ductal adenocarcinomas" of the pancreas. The fundamental DNA (genetic) changes that underlie the development of acinar cell carcinomas have not yet been elucidated. Scientists at Johns Hopkins studied 21 acinar cell carcinomas of the pancreas and found a distinct pattern of DNA changes in these tumors. These DNA changes included loss of chromosome arm 11p and changes in the "APC/beta-catenin pathway." These results indicate that acinar cell carcinomas are genetically distinct from pancreatic ductal adenocarcinomas, but some cases contain genetic alterations common to another rare tumor type in the pancreas called "pancreatoblastomas." An understanding of the variants of pancreatic cancer helps us understand why some tumors occur in different patients. In addition, it should form a basis for targeting specific therapies to specific tumor types.
American Journal of Pathology (Volume 160,pages 953-962)
Discovery of a panel of genes made by pancreatic cancers (February and March 2002)
Scientists at Johns Hopkins used two different techniques―"SAGE" and gene chips―to discover a panel of over 100 genes that are made at high levels in pancreatic cancer but not in normal tissues. They used the recently developed technology "SAGE" (serial analysis of gene expression) technology as well as cutting-edge gene chips. These technologies were applied to a panel of pancreatic cancers and normal pancreas cells and the investigators discovered a novel panel of over genes that appear to be made ("expressed") at high levels in pancreatic cancer. Several genes that may be involved in the fundamental nature of malignant changes in pancreatic ductal epithelium were identified. Some genes, such as S100A4, prostate stem cell antigen, and carcinoembryonic antigen-related cell adhesion molecule 6, suggest potential use as diagnostic markers. Others suggest potential novel therapeutic targets. These two studies provide insight into the fundamental nature of pancreatic cancer and each of the more than 100 genes discovered to be made at high levels in pancreatic cancer may serve as a new marker for the early detection of pancreatic cancer, or as a target for the development of new chemotherapies.
Cancer Research (Volume 62, pages 819-826)
American Journal of Pathology (Volume 160, pages 1239-1249)
Target of chemopreventive agents made in pancreatic cancer precursors
One of the more exciting approaches to saving lives that would otherwise be lost to pancreatic cancer is preventing pancreatic cancer through the use of "chemopreventive" agents. Chemopreventive agents are drugs that are taken regularly and reduce one's risk of cancer. For example, a recent study suggested that regular aspirin use may reduce the risk of developing pancreatic cancer. Cox-2 (also known as cyclooxygenase 2) is an enzyme made by cells that is a target for some chemopreventive drugs. In the August issue of the American Journal of Clinical Pathology Dr. Maitra and colleagues from Johns Hopkins report that cyclooxygenase 2 is expressed (made by) small lesions in the pancreas called "pancreatic intraepithelial neoplasia".
Why is this important?
Pancreatic intraepithelial neoplasia is believed to be the precursor to pancreatic cancer. The expression of cyclooxygenase 2 in pancreatic intraepithelial neoplasia lesions suggests that cyclooxygenase 2 inhibitors could be used to prevent the development of pancreatic cancer. Further work is needed, but clearly chemopreventive agents, such as cyclooxygenase 2 inhibitors, offer an exciting new approach to fight pancrewatic cancer before it develops.
Am J Clin Pathol 2002 Aug;118(2):194-201.
BRCA2 gene important in familial pancreatic cancer
In the July 2002 issue of Cancer research K. Murphy and colleagues from Johns Hopkins reported that 1 in 6 (17%) patients with a very strong family history of pancreatic cancer have inherited ("germline") mutations (changes) in the BRCA2 gene. The BRCA2 is also known as the second breast cancer gene. Although it has been known for years that BRCA2 was important in familial breast cancer, the importance of BRCA2 in familial pancreatic cancer is only now coming to light. Inherited mutations in BRCA2 are particularly common in the Askenazi Jewish population.
Why is this important?
The identification of a gene responsible for the familial aggregation of pancreatic cancer is important because at-risk family members can now be tested to see if they carry this gene. If you are interested in learning more about genetic testing visit: https://www.pbs.org/gene/findout/3_findout.html. To find a genetic counselor near you visit: https://www.nsgc.org/. To join the National Familial Pancreas Tumor Registry at Johns Hopkins, contact Alison Klein: [email protected].
Cancer Res 2002 Jul 1;62(13):3789-93.
Genetic alterations in solid-pseudopapillary tumors of the pancreas
Solid-pseudopapillary tumors are rare tumors of the pancreas that arise primarily in young women. They have a distinct appearance under the microscope and a much much better prognosis than the more common ductal adenocarcinomas of the pancreas. Dr. Susan Abraham and colleagues studied the fundamental genetic (DNA) changes in a series of solid-pseudopapillary tumors of the pancreas and found that they almost all have mutations (DNA changes) in a particular gene called Beta-catenin. By contrast, usual ductal adenocarcinomas of the pancreas almost never have Beta-catenin mutations.
Why is this important?
It can sometimes be difficult in a small biopsy or even in a resected specimen to distinguish between the various types of tumors that arise in the pancreas. This discovery by Dr. Abraham suggests that the presence or absence of Beta-catenin mutations in a tumor can be used to distinguish between solid-pseudopapillary tumors (which have a very good prognosis) and usual ductal adenocarcinomas (which do not have a good prognosis)
Am J Pathol 2002 Apr;160(4):1361-9
Genetic alterations in acinar cell carcinomas of the pancreas
Acinar cell carcinomas are rare malignant tumors of the pancreas. They are microscopically different from the more common "ductal adenocarcinomas" of the pancreas. The fundamental DNA (genetic) changes that underlie the development of acinar cell carcinomas have not yet been elucidated. Scientists at Johns Hopkins studied 21 acinar cell carcinomas of the pancreas and found a distinct pattern of DNA changes in these tumors. These DNA changes included loss of chromosome arm 11p and changes in the "APC/beta-catenin pathway". These results indicate that acinar cell carcinomas are genetically distinct from pancreatic ductal adenocarcinomas, but some cases contain genetic alterations common to another rare tumor type in the pancreas called "pancreatoblastomas".
Why is this important?
An understanding of the variants of pancreatic cancer helps us understand why some tumors occur in different patients. In addition, it should form a basis for targeting specific therapies to specific tumor types.
Am J Pathol 2002 Mar;160(3):953-62
Discovery of a panel of genes made by pancreatic cancers
Scientists at Johns Hopkins used two different techniques- "SAGE" and gene chips to discover a panel of over 100 genes that are made at high levels in pancreatic cancer but not in normal tissues. Dr. Ryu and colleagues used the recently developed technology "SAGE" (serial analysis of gene expression) technology while Dr. Christine Iacobuzio-Donahue and colleagues used gene chips. These technologies were applied to a panel of pancreatic cancers and normal pancreas cells and Drs. Ryu and Iacobuzio-Donahue discovered a novel panel of over genes that appear to be made ("expressed") at high levels in pancreatic cancer. Several genes that may be involved in the fundamental nature of malignant changes in pancreatic ductal epithelium were identified. Some genes, such as S100A4, prostate stem cell antigen, carcinoembryonic antigen-related cell adhesion molecule 6, and mesothelin, suggest potential use as diagnostic markers. Others suggest potential novel therapeutic targets.
Why is this important?
These two studies provide insight into the fundamental nature of pancreatic cancer and each of the more than 100 genes discovered to be made at high levels in pancreatic cancer may serve as a new marker for the early detection of pancreatic cancer, or as a target for the development of new chemotherapies.
Cancer Res 2002 Feb 1;62(3):819-26
Am J Pathol. 2002 Apr;160(4):1239-49
Extent of surgery for pancreatic cancer:
The extent of surgery appropriate for patients with pancreatic cancer has long been debated. Some surgeons perform a "standard" whipple resection (also called a standard pancreaticoduodenectomy) while others have suggested that more extensive ("radical") surgery is needed. Dr. C. Yeo and colleagues from Johns Hopkins therefore performed a randomized study of 294 patients surgically treated at Johns Hopkins. Patients were randomized to either a "standard" whipple or a more "radical" whipple procedure. In the September 2002 issue of the Annals of Surgery, Dr. Yeo reports that the radical (extended) whipple can be performed with similar mortality (death rate) but some increased morbidity (complications) compared to standard whipple. No long-term benefit was found in the more radical surgery.
Why is this important?
This study suggests that although more radical surgery can be performed safely, it may not provide any long-term benefits.
Ann Surg 2002 Sep;236(3):355-68
2001 ▼
New marker for pancreatic cancer (December 2001)
Researchers at Johns Hopkins identified a new marker for pancreatic cancer. This marker was discovered using "SAGE" a technology developed at Johns Hopkins to help scientists determine which genes are expressed (made) by a cancer. Dr. Argani found that almost all pancreatic cancers express the gene called "mesothelin" at levels much higher than those found in normal, non-cancerous, tissues. The discovery that mesothelin is made at high levels in pancreatic cancer has potential diagnostic, imaging, and therapeutic implications. For example, scientists in Dr. Liz Jaffee's lab are already conducting studies in the laboratory to see if mesothelin can be used as an immune target to treat patients with pancreatic cancer.
Clinical Cancer Research (Volume 7, pages 3862-3868)
New prognostic marker for pancreatic cancer (December 2001)
It can be very hard to predict the prognosis for patients with pancreatic cancer. Dr. M. Tascilar and colleagues at Johns Hopkins studied 249 patients with pancreatic cancer who underwent a Whipple resection for pancreatic cancer. Patients with pancreatic cancers that expressed (made) the SMAD4 protein had significantly longer survival (19.2 months) than did patients whose cancers did not express (make) the SMAD4 protein (14.7 months). This SMAD4 survival benefit persisted after adjustment for known prognostic factors including tumor size, margins, lymph node status, pathological stage, blood loss, and use of adjuvant chemoradiotherapy. From this, Dr. Tascilar was able to conclude that patients undergoing Whipple resection for pancreatic cancer survive longer if their cancers express SMAD4.
This study helps confirm the importance of the SMAD4 gene in pancreatic cancer.
Clinical Cancer Research (Volume 7, pages 4115-4121)
Unraveling the genetic changes in pancreatoblastomas (August 2001)
While scientists have made great strides in advancing our understanding of pancreatic ductal adenocarcinoma, little is known about rare tumors that arise in the pancreas. Pancreatoblastoma is a rare pancreatic tumor with a distinctive microscopic appearance that generally affects infants and young children. Researchers at Johns Hopkins analyzed a series of nine pancreatoblastomas for genetic alterations (changes in the DNA sequence of the tumors). They found three interesting things. First, pancreatoblastomas are genetically very different from the more common ductal adenocarcinomas of the pancreas. Pancreatoblastomas show alterations (mutations) in the beta-catenin/APC genes. Second, they also showed that chromosome 11p is frequently altered in pancreatoblastomas. Chromosome 11p is frequently altered in hepatoblastomas (a rare pediatric tumor in the liver), suggesting that pancreatoblastomas are more closely related to hepatoblastomas than they are to pancreatic ductal adenocarcinomas. Finally, one of the patients included in the series of pancreatoblastomas had the clinical syndrome called "familial adenomatous polyposis" or "FAP." Patients with familial adenomatous polyposis develop numerous polyps in their colon at an early age and this study demonstrates that they can also develop pancreatoblastomas. An understanding of the variants of pancreatic cancer helps us understand why some tumors occur in adults and some in children. In addition, it should form a basis for targeting specific therapies to specific tumor types.
American Journal of Pathology (Volume 150, pages 1619-1627)
Markers of cancer invasion (July 2001)
There is a great effort underway to identify new ways to detect cancers early. A major approach is to identify "tumor-specific" and "tissue-specific" markers. For example, useful markers can be substances found to be produced by cancer cells in both tissue culture (cancer cells grown artificially outside the body) and in patient samples. Such markers would not be normally found in normal tissues at a high level. These are the invasion-specific markers. Dr. Ryu and colleagues in Dr. Kern's laboratory for pancreatic cancer research at Johns Hopkins searched for such genes. Dozens of invasion-specific markers were identified in invasive cancers obtained from patient samples. Many of these were new markers not previously considered as cancer markers and many of the genes are expressed not by the tumor cells but instead by the patient's response to the tumors. Some of these markers are known to be secreted and to be detectable in simple blood samples. A strong effort is underway to examine these candidates and develop markers for use in the early detection of cancer, to aid medical imaging and to serve as targets for the development of invasion-specific anticancer therapy.
Cancer Research (Volume 61, pages 1833-8)
Activin receptors-A new anticancer signal in human tumors (June 2001)
The major problem with human tumors is that they do not obey the signals from their surrounding cells that should restrain their growth. To date, very few of such signals have been defined, and this limits our ability to understand and counter this basic abnormality. Because we need to understand these signals, there has been a great effort to identify genes that are mutated and turned off in tumors. These are the "tumor-suppressor genes." The inactivation of these genes allows tumors to escape from the normal growth controls that the surrounding cells and tissue are trying to place on them. Activin is a protein secreted by normal cells. To exert its action, it must bind receptors on a cell.
The receptors propagate a signal to the cell but it was not previously known that these signals were able to suppress tumor growth. Mutations within the activin receptor gene were found in some pancreatic and biliary cancers by Dr. Gloria Su and colleagues in Dr. Kern's laboratory for pancreatic cancer research at Johns Hopkins. In tumors that lack the mutations, someday it might be possible to administer activin as a therapeutic strategy. It might also be possible to mimic the effects of activin on tumor cells by a precise molecular targeting using specially designed new drugs that directly activate the signal pathway without the need for intact receptors. This is a new idea that was previously unknown, but now can be explored. It is our hope that one can design a therapy to attack the most vulnerable components of pancreatic cancer.
Proc Natl Acad Sci USA (Volume 98, pages 3254-7)
Hopkins' scientists use molecular tool to discover new markers of hepatopancreatico-biliary cancer (June 2001)
Dr. Argani and colleagues from Johns Hopkins discover a new marker of pancreatic cancer. This new marker called "prostate stem-cell antigen" (PSCA) was discovered by using a technique developed at Johns Hopkins called "serial analysis of gene expression" (SAGE). Since the original description of SAGE, a group of cooperating scientists from a number of institutions have created an online database of gene expression that includes SAGE data on a variety of tissues and cancers (https://www.ncbi.nlm.nih.gov/SAGE/). The investigators at Johns Hopkins used this database to compare the gene expression levels in pancreatic cancer tissues with those seen in non-cancerous pancreatic tissues. The goal was to identify genes selectively "turned-on" in the cancers. One of the genes found using this approach is called "prostate stem-cell antigen." Prostate stem-cell antigen is a gene originally thought to be largely restricted to prostate cells. Dr. Argani and colleagues demonstrate that prostate stem-cell antigen (PSCA) is, in fact, highly overexpressed in approximately 60% of primary pancreatic cancers. It is not expressed in the normal pancreas. These findings are exciting for several reasons. First, they demonstrate the power of new technologies such as SAGE to discover new tumor markers. Second, PSCA, because it is selectively overexpressed in pancreatic cancers, might be a useful marker for pancreatic cancer. Third, other groups have shown that PSCA can be an immune target and therefore PSCA is being explored as a target for the immune treatment of cancers. The demonstration of PSCA expression in pancreatic cancer suggests a new avenue for treating pancreatic cancers, immunotherapy directed at cells expressing PSCA.
Cancer Research (Volume 61, pages 4320-4324)
Molecular and immunohistochemical analysis of small cell carcinoma of the gallbladder: An unusual entity (May 2001)
Dr. Argani and colleagues published the largest series of cases examining small cell carcinomas of the gallbladder, a highly unusual neoplasm that has been described only recently. Dr. Maitra characterized the clinical, histopathologic, immunohistochemical and molecular features of 12 small cell carcinomas of the gallbladder. It was discovered that only half of these rare cancers are "pure" and half are combined with other neoplasms (e.g., adenocarcinoma, squamous carcinoma, and rarely, carcinosarcoma). These cancers were studied using molecular and immunohistochemical techniques. We found that the molecular changes in small cell carcinomas were similar to those of adenocarcinomas occurring at this site, with a high frequency of p53 and p16INK4a abnormalities, and a low frequency of deleted in pancreatic carcinoma-4 (Dpc-4) inactivation and K-ras codon 12 mutations. In contrast to small cell carcinomas of the lung, p16INK4a function appears to be abrogated more frequently in these carcinomas. We hope these results will help us develop a rational approach to the diagnosis and therapy of these unusual tumors.
American Journal of Surgical Pathology (Volume 25, pages 595-601)
Molecular analysis of bile duct carcinomas (April 2001)
Using immunohistochemical labeling, Dr. Argani and colleagues were able to show that the DPC4, a tumor suppressor gene discovered at Johns Hopkins that is known to play a major role in pancreatic cancer, is also targeted in bile duct carcinomas. Loss of Dpc4 protein was identified in a significant percentage of bile duct carcinomas. However, not all bile duct carcinomas were equal: we were able to demonstrate that distal common bile duct carcinomas (those located near the pancreas) were far more likely to demonstrate loss of DPC4 than proximal bile duct cancers (Klatskin tumors and cholangiocarcinomas of the liver). In fact, the frequency of DPC4 loss that we demonstrated in distal bile duct carcinomas (55%) is identical to that which was demonstrated in pancreatic cancer. Similarly, we were able to show that the p53 gene product was abnormally expressed far more frequently in distal bile duct cancers than proximal ones. These results show that distal common bile duct cancers have some of the same genetic alterations as pancreatic cancers, while other bile duct cancers are biologically distinct. We hope that these results will allow us to develop more rational therapies for these tumors.
Cancer (Volume 91, pages 1332-1341)
Familial pancreatic cancer (March 2001):
For years, isolated reports in the medical literature have suggested that pancreatic cancer runs in some families. For example, it has been reported that former President Jimmy Carter lost his father, two sisters and brother to pancreatic cancer. A. Tersmette and colleagues from Johns Hopkins report that first-degree relatives (brothers and sisters, parents and children) of patients with "familial pancreatic cancer" have a significantly increased risk of developing pancreatic cancer. Tersmette and colleagues followed 341 families enrolled in the National Familial Pancreas Tumor Registry (NFPTR) and found that the first-degree relatives of familial pancreatic patients had an 18-fold increased risk of developing pancreatic cancer when compared to the general population (the "SEER" database). In this study, familial pancreatic cancer was defined as at least a pair of first-degree relatives with pancreatic cancer in a family. Remarkably, if there were three or more family members with pancreatic cancer when the family enrolled in the NFPTR, then the risk of other family members developing pancreatic cancer jumped to 57-fold greater than the general population. This study firmly establishes that "Familial Pancreatic Cancer" is a real entity and it provides a quantitative measure of the risk of pancreatic cancer in these families. Studies such as this will form the basis for identifying individuals at-risk for developing pancreatic cancers who might benefit from new screening tests as they are developed.
Clinical Cancer Research (Volume 7, pages 738-744)
New vaccine to treat pancreatic cancer (January 2001)
Dr. Elizabeth Jaffee and colleagues at Johns Hopkins report the result of a phase I clinical trial of a novel vaccine treatment for patients with a pancreatic cancer. The vaccine was produced by genetically altering pancreatic cancer cells growing in culture so that the cells would produce large quantities of an immune activating factor called "Granulocytic-macrophage colony-stimulating factor" (or GM-CSF for short). Dr. Jaffee treated 14 patients with this vaccine in a phase I dose escalation trial. The patients underwent surgery at Johns Hopkins after which they received various doses of the vaccine. No dose-limiting toxicities were encountered. Instead, Dr. Jaffee was able to demonstrate that the vaccine induced an anti-tumor immune response in three patients who received the highest dose of the vaccine (>10x107 vaccine cells). Remarkably, these three patients remained alive and free of disease more than 36 months after diagnosis. Based on these results, Dr. Jaffee and her team will conduct phase II trials of the GM-CSF vaccine. These trials are scheduled to begin in the late summer.
The Journal of Clinical Oncology (Volume 19, pages 145-156)
Consistent overexpression of Fatty Acid Synthase (FAS) in biliary tract carcinomas: A novel target for anti-biliary tract cancer drug development (January 2001):
Fatty Acid Synthase (FAS) is the primary enzyme involved in the breakdown of fats. FAS has been demonstrated to be overexpressed in several human cancers (breast, endometrial, prostate, colon). In some cancers, high levels of FAS expression have been associated with poor prognosis, suggesting that FAS expression may promote tumor growth and virulence. Recently synthesized inhibitors of FAS have demonstrated antitumor activity without concurrent toxicity to normal tissues, and hence hold promise as therapy for tumors that overexpress FAS (Cancer Res 2000; 60: 213-218) (PNAS 2000; 97: 3450-3454). FAS expression had not been studied in biliary tract carcinomas, which are highly aggressive and often do not respond to conventional therapy. Dr. Argani and colleagues recently examined 107 biliary tract carcinomas for FAS overexpression using an immunohistochemical assay on formalin-fixed, paraffin-embedded tissue. FAS was overexpressed in 93% of carcinomas of the biliary tract. Therefore, FAS inhibitors hold promise as a new therapy for biliary tract carcinomas.
Modern Pathology (Volume 14, page 192A)
New Marker for pancreatic cancer
In the December 2001 issue of Clinical Cancer Research Dr. Argani and colleagues from Johns Hopkins reported the identification of a new marker for pancreatic cancer. This marker was discovered using "SAGE" a technology developed at Johns Hopkins to help scientists determine which genes are expressed (made) by a cancer. Dr. Argani found that almost all pancreatic cancers express the gene called "mesothelin" at levels much higher than those found in normal, non-cancerous, tissues.
Why is this important?
The discovery that mesothelin is made at high levels pancreatic cancer has potential diagnostic, imaging, and therapeutic implications. For example, scientists in Dr. Liz Jaffee's lab are already conducting studies in the laboratory to see if mesothelin can be used as an immune target to treat patients with pancreatic cancer.
Clin Cancer Res 2001 Dec;7(12):3862-8
New prognostic marker for pancreatic cancer
It can be very hard to predict the prognosis for patients with pancreatic cancer. Dr. M. Tascilar and colleagues at Johns Hopkins studied 249 patients with pancreatic cancer who underwent a Whipple resection for pancreatic cancer. Patients with pancreatic cancers that expressed (made) the SMAD4 protein had significantly longer survival (19.2 months) than did patients whose cancers did not express (make) the SMAD4 protein (14.7 months). This SMAD4 survival benefit persisted after adjustment for known prognostic factors including tumor size, margins, lymph node status, pathological stage, blood loss, and use of adjuvant chemoradiotherapy. From this, Dr. Tascilar was able to conclude that patients undergoing Whipple resection for pancreatic cancer survive longer if their cancers express SMAD4.
Why is this important?
This study helps confirm the importance of the SMAD4 gene in pancreatic cancer. While SMAD4 may be useful as a marker for prognosis, one should always keep in mind, as stated by Stephen Jay Gould, that "the median isn't the message".
Clin Cancer Res 2001 Dec;7(12):4115-21
Unraveling the genetic changes in pancreatoblastomas
While scientists have made great strides in advancing our understanding of pancreatic ductal adenocarcinoma, little is known about rarer tumors that arise in the pancreas. Pancreatoblastoma is a rare pancreatic tumor with a distinctive microscopic appearance that generally affects infants and young children (click here for more information on pancreatoblastomas and other rarer variants of pancreas cancer). Dr. Abraham analyzed a series of nine pancreatoblastomas for genetic alterations (changes in the DNA sequence of the tumors). She found three interesting things. First, pancreatoblastomas are genetically very different from the more common ductal adenocarcinomas of the pancreas. Pancreatoblastomas show alterations (mutations) in the beta-catenin/APC genes. 2) Dr. Abraham also showed that chromosome 11p is frequently altered in pancreatoblastomas. Chromosome 11p is frequently altered in hepatoblastomas (a rare pediatric tumor in the liver), suggesting that pancreatoblastomas are more closely related to hepatoblastomas than they are to pancreatic ductal adenocarcinomas. 3) Finally, one of the patients included in Dr. Abraham's series of pancreatoblastomas had the clinical syndrome called "familial adenomatous polyposis" or "FAP". Patients with familial adenomatous polyposis develop numerous polyps in their colon at an early age and Dr. Abraham demonstrates that they can also develop pancreatoblastomas.
Why is this important?
An understanding of the variants of pancreatic cancer helps us understand why some tumors occur in adults and some in children. In addition, it should form a basis for targeting specific therapies to specific tumor types.
American Journal of Pathology 159:1619-1627, 2001
Markers of Cancer Invasion
In an effort to identify new ways to identify cancers that otherwise would remain undetected for too long, Dr. Ryu and colleagues in Dr. Kern's laboratory for pancreatic cancer research at Johns Hopkins searched for genes ("markers") produced by the invasive tumor or the body's reaction to it. Dozens of invasion-specific markers were identified in invasive pancreatic cancers obtained from patient samples. Many of these were new markers not previously considered as cancer markers, and many of the genes are expressed not by the tumor cells but instead by the patient's response to the tumors. Some of these markers are known to be secreted and to be detectable in simple blood samples.
Why is this important?
A strong effort is underway to examine these candidate genes and to develop markers for use in reliable assays for cancer that can be done on serum, to aid medical imaging, and to serve as targets for the development of invasion-specific anticancer therapy.
Cancer Res 61: 1833-1838, 2001
Activin Receptors - A New Anticancer Signal in Human Tumors
The major problem with human tumors is a social one. Tumor cells do not obey the signals from their surrounding cells that should restrain their growth. To date, very few of such signals have been defined, and this limits our ability to understand and counter this basic abnormality.
Because of the need to understand these signals, there has been a great effort to identify genes that are mutated and turned off in tumors. These are the tumor-suppressor genes. The inactivation of these genes allows tumors to escape from the normal growth controls that the surrounding cells and tissue are trying to place on them.
Activin is a protein secreted by normal cells. To exert its action, activin must bind receptors on a cell. The receptors propagate a signal to the cell, but it was not previously known that these signals were able to suppress tumor growth. Mutations within the activin receptor gene were found recently in some pancreatic cancers by Dr. Gloria Su and colleagues in Dr. Kern's laboratory for pancreatic cancer research at Johns Hopkins.
Why is this important?
In tumors that lack the mutations, someday it might be possible to administer activin as a therapeutic strategy. It might also be possible to mimic the effects of activin on tumor cells by a precise molecular targeting using specially designed new drugs that directly activate the signal pathway without the need for intact receptors. This is a new idea that was previously unknown, but now can be explored. It is our hope that one can design a rational therapy that would specifically attack the most vulnerable components of pancreatic cancer.
Proc Natl Acad Sci USA. 98: 3254-3257, 2001
Discovery of New Markers of Pancreatic Cancer
In the June 1st issue of Cancer Research Dr. Argani and colleagues from Johns Hopkins described the discovery of a new marker of pancreatic cancer. This new marker called "prostate stem-cell antigen" (PSCA) was discovered by using a technique developed at Johns Hopkins called "serial analysis of gene expression". Since the original description of SAGE, a group of cooperating scientists from a number of institutions have created an online database of gene expression that includes SAGE data on a variety of tissues and cancers (www.ncbi.nlm.nih.gov/SAGE/). The investigators at Hopkins used this database to compare the gene expression levels in pancreatic cancer tissues with those seen in non-cancerous pancreatic tissues. The goal was to identify genes that were selectively "turned-on" in the cancers. One of the genes the Hopkins found using this approach coded for a protein called "prostate stem-cell antigen." Prostate stem-cell antigen is a gene that was originally thought to be largely restricted to prostate cells. Dr. Argani and colleagues demonstrate that prostate stem-cell antigen (PSCA) is, in fact, highly overexpressed in approximately 60% of primary pancreatic cancers. It is not expressed in the normal pancreas.
Why is this important?
These findings are exciting for several reasons. First, they demonstrate the power of new technologies such as SAGE to discover new tumor markers. Second, PSCA, because it is selectively overexpressed in pancreatic cancers, maybe a useful marker for pancreatic cancer. Third, other groups have shown that PSCA can be an immune target and therefore PSCA is being explored as a target for the immune treatment of cancers. The demonstration of PSCA expression in pancreatic cancer suggests a new avenue for treating pancreatic cancers. That is, immunotherapy directed at cells expressing PSCA.
On an important side note, this work was supported, in large part, by generous donations from the friends and family of Michael Rolfe demonstrating the power of private giving to advance pancreatic cancer research.
Cancer Research 61:4320-4324, 2001.
(https://aacrjournals.org/cancerres/article/61/11/4320/507556/Discovery-of-New-Markers-of-Cancer-through-Serial)
Familial Pancreatic Cancer
For years, isolated reports in the medical literature have suggested that pancreatic cancer runs in some families. For example, it has been reported that former President Jimmy Carter lost his father, brother and two sisters from pancreatic cancer.
Tersmette and colleagues from Johns Hopkins report that first-degree relatives (brothers and sisters, parents and children) of patients with "familial pancreatic cancer" have a significantly increased risk of developing pancreatic cancer. Tersmette and colleagues followed 341 families enrolled in the National Familial Pancreas Tumor Registry (NFPTR) at Johns Hopkins and found that the first-degree relatives of familial pancreatic patients had an 18-fold increased risk of developing pancreatic cancer when compared to the general population (the "SEER" database). In this study, familial pancreatic cancer was defined as at least a pair of first-degree relatives with pancreatic cancer in a family. Remarkably, if there were three or more family members with pancreatic cancer when the family enrolled in the NFPTR, then the risk of other family members developing pancreatic cancer jumped to 57-fold greater than the general population.
Why is this important?
This study firmly establishes that "Familial Pancreatic Cancer" is a real entity and it provides a quantitative measure of the risk of pancreatic cancer in these families. Importantly, studies such as this will form the basis for identifying individuals at-risk for developing pancreatic cancer who might benefit from new screening tests as they are developed.
If you have a strong family history of pancreatic cancer and would like to join the research studies currently underway at Hopkins, please consider joining the NFPTR. If you would like to join, please contact the Coordinator of the NFPTR, Mirian Tillery.
Clin Cancer Res 7:738-744, 2001
(https://aacrjournals.org/clincancerres/article/7/3/738/200023/Increased-Risk-of-Incident-Pancreatic-Cancer-Among)
New Vaccine to Treat Pancreatic Cancer
In the January issue of The Journal of Clinical Oncology (volume 19; 2001: pages 145-156), Dr. Elizabeth Jaffee and colleagues at Johns Hopkins reported the result of a phase I clinical trial of a novel vaccine treatment for patients with a pancreatic cancer. The vaccine was produced by genetically altering pancreatic cancer cells growing in culture so that the cells would produce large quantities of an immune activating factor called "Granulocytic-macrophage colony-stimulating factor" (or GM-CSF for short). Dr. Jaffee treated 14 patients with this vaccine in a phase I dose escalation trial. The patients underwent surgery at Hopkins after which they received various doses of the vaccine. No dose-limiting toxicities were encountered. Instead, Dr. Jaffee was able to demonstrate that the vaccine induced an anti-tumor immune response in three patients who received the highest dose of the vaccine (>10x107 vaccine cells). Remarkable, these three patients remained alive and free of disease more than 25 months after diagnosis.
Why is this important?
Based on these results, Dr. Jaffee and her team are conducting phase II trials of the GM-CSF vaccine. As much as Dr. Jaffee would like to offer the vaccine to everyone, eligibility criteria had to be established for this study. Patients with adenocarcinoma of the pancreas who have surgery Johns Hopkins Hospital to remove their pancreas cancer and who have no clinical evidence of spread of the cancer outside the pancreas will be eligible for this study. Patients with bile duct cancer or neuroendocrine tumors or islet cell cancer are not eligible. Please contact Dr. Elizabeth Jaffee or Barbara Biedrzycki, R.N. for more information on eligibility criteria.
The Journal of Clinical Oncology 19:145-156, 2001
2000 ▼
Genes isolated from Tumor Vessels:
Dr. St. Croix in Bert Vogelstein and Kern Kinzler's laboratory identified 46 genes which appear to be specifically elevated (or "turned on") in tumor-associated blood vessels.
Why is this important?
The identification of these genes is exciting because they are potential targets for drugs aimed at shrinking tumors by starving them of their blood supply.
Science 289:1121-2,2000
Thousands of Chemical Compounds Tested
Drs. Gloria Su and Taylor Sohn in Scott Kern's laboratory tested over 16,000 chemical compounds looking for compounds that can "turn on" on a specific function that is often "broken "in pancreatic cancer (DPC4 signaling pathway). They identified half a dozen promising compounds, one of which turned out to be a novel and specific inhibitor of a protein called HDAC (histone deacetylase).
Why is this important?
This finding represents a new method to develop drugs to treat pancreatic cancer - "fixing" the cancer cells by screening for compounds that turn on specific functions lost in the cancer.
Gene Inactivation in Precursors to Invasive Pancreatic Cancer
Drs. Michael Goggins and Robb Wilentz studied the genetic changes in the very earliest lesions that give rise to invasive pancreatic cancer. They found that the BRCA2 and DPC4 genes are inactivated in some of these early lesions (called "Pancreatic Intraepithelial Neoplasia").
Why is this important?
These studies provide an important first step in the development of novel screening tests to detect early, and therefore potentially curable, pancreatic cancers.
Am J Pathol 156:1641-1651,2000
Cancer Research 60:2002-2006,2000
DNA Methylation in Pancreatic Cancer
Dr. T. Ueki in Michael Goggins' laboratory discovered that a number of genes are selectively "hypermethylated" in pancreatic cancer. Methylation refers to the addition of an extra carbon atom to DNA and it is a common mechanism by which cancer preventing genes (tumor-suppressor genes) are inactivated in cancers.
Why is this important?
These findings provide a novel target for the development of a new screening test for pancreatic cancer.
Cancer Research 60:1835-1839,2000.
Quality of Life After a Whipple
Drs. Taylor Sohn and Charles Yeo studied patients' self-reported quality of life after Whipple surgery (pancreaticoduodenectomy). Over 192 patients were studied and over 30 quality of life measurements assayed. Remarkably, quality of life scores for patients who underwent a Whipple at Johns Hopkins were comparable to those patients who had their gallbladder removed for stones.
Why is this important?
These data demonstrate that surviving Whipple patients as a group have near normal quality of life scores. This corrects the misimpression that Whipple patients have severely impaired quality of life, and cannot return towards normal activities.
Journal of Gastrointestinal Surgery 4:355-365,2000
New Immunohistochemical Stain for the DPC4 Gene Product
In 1996, Dr. Scott Kern and colleagues at Hopkins discovered a new gene which appeared to be selectively inactivated (deleted) in the development of cancer of the pancreas. Dr. Kern and his colleagues named this gene "DPC4" for Deleted in Pancreas Cancer locus 4 (see Science 1996, vol. 271:350-353). The discovery of this gene was exciting because DPC4 is inactivated in a large number of cancers of the pancreas, and because its inactivation appears to be relatively specific for cancer of the pancreas. That is, DPC4 appears to be only rarely inactivated in other tumor types (see Cancer Research 1996, vol 56:2527-2530).
Robb Wilentz and colleagues from Johns Hopkins developed a new immunohistochemical stain for DPC4. This new stain can detect DPC4 in tissue sections (such as biopsies), and the staining pattern directly mirrors the DPC4 gene status.
Why is this important?
Because of its simplicity and availability, the immunohistochemical staining technique Dr. Wilentz developed for DPC4 has a number of direct clinical applications. For example, staining for DPC4 may help to distinguish benign chronic pancreatitis (which should express DPC4) from cancer of the pancreas (half of which will not express DPC4). Thus, DPC4 staining will add a valuable tool to the interpretation of needle biopsies of the pancreas. In addition, the immunohistochemical assay reported by Wilentz and colleagues for DPC4 may lead to answers in the investigative area. For instance, the immunohistochemical study of early lesions in the pancreas may help determine the stage at which DPC4 inactivation contributes to neoplastic progression and thereby help in the development of new screening tests for early pancreatic cancer.
American Journal of Pathology 156:37-43,2000